Dumping syndrome is a condition characterized by rapid gastric emptying, leading to a range of symptoms after eating, particularly following certain types of weight loss surgeries, including gastric sleeve surgery. There are two main types of dumping syndrome: early dumping, which occurs within 30 minutes after eating, and late dumping, which happens 1 to 3 hours post-meal. The condition is caused by the swift passage of food from the stomach into the small intestine, often exacerbated by high-sugar or high-fat meals. Patients who undergo gastric sleeve surgery are at an increased risk for developing dumping syndrome due to the altered anatomy and reduced stomach size. Symptoms may include nausea, vomiting, abdominal cramps, diarrhea, dizziness, and rapid heart rate. Management strategies for dumping syndrome typically involve dietary modifications, such as eating smaller, more frequent meals, avoiding sugars and simple carbohydrates, and incorporating high-protein foods. In some cases, medications may be prescribed to alleviate symptoms.
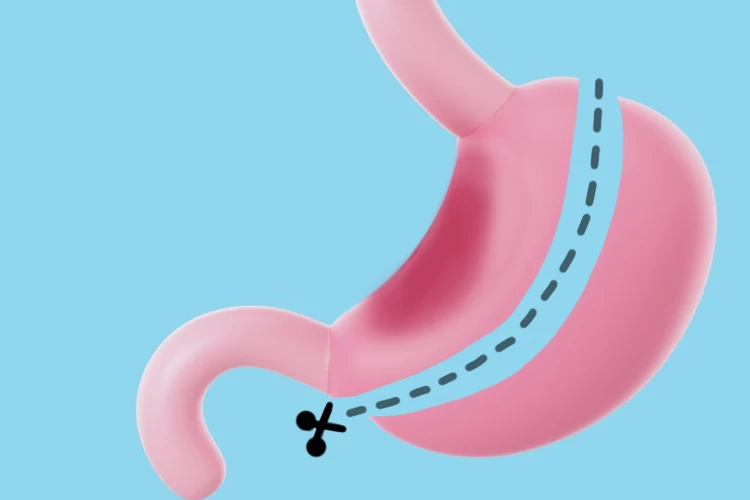
Gastric sleeve surgery, also known as sleeve gastrectomy, is a bariatric procedure that involves removing a large portion of the stomach, creating a smaller, tube-shaped stomach. This restricts food intake, leading to weight loss. It's used to treat obesity and related conditions like type 2 diabetes, hypertension, and sleep apnea. The procedure is typically laparoscopic (minimally invasive), with patients experiencing several days of hospitalization and a recovery period involving dietary restrictions and lifestyle adjustments. Post-operative care includes regular follow-up appointments to monitor weight loss, nutritional status, and overall health. Gastric sleeve surgery typically results in a 60-70% reduction of excess body weight within 12-18 months. Individual results vary based on factors like adherence to post-operative guidelines and individual metabolism.
Laparoscopic Sleeve Gastrectomy (LSG) is a minimally invasive weight-loss surgery that involves the removal of a significant portion of the stomach, resulting in a sleeve-like structure that restricts food intake. The procedure is done under general anesthesia through small cuts in the abdomen using special instruments. It’s typically recommended for people with a body mass index (BMI) of 40 or higher, or those with a BMI of 35 or higher who have obesity-related health conditions. While LSG can lead to significant weight loss and health improvements, there are risks involved, such as infection, bleeding, leaks from the new stomach sleeve, and nutritional deficiencies. Careful patient selection and follow-up care are important for a successful recovery.
Weight gain after gastric sleeve surgery can occur due to various factors, despite the procedure's initial effectiveness in promoting weight loss. Common causes include poor dietary choices, such as consuming high-calorie, sugary, or processed foods, which can lead to overeating and the stretching of the stomach pouch. Psychological factors, such as emotional eating, can also contribute to weight regain. Additionally, metabolic adaptations and lifestyle changes post-surgery may impact weight management. To address these issues, solutions include adopting a balanced, nutrient-dense diet, engaging in regular physical activity, and seeking support through counseling or support groups. Monitoring portion sizes and practicing mindful eating are also crucial in maintaining weight loss and preventing regain after gastric sleeve surgery.