Infections after Dental Implant Surgery: Causes & Treatments
Dental Care
Tooth implant infection is a serious complication that can occur following dental implant surgery. While dental implants are generally considered a safe and effective way to replace missing teeth, infections can sometimes develop if proper oral hygiene is not maintained or if there are underlying health issues. If not promptly treated, these infections can lead to pain, swelling, and even the loss of the implant. Treatments for tooth implant infection may involve the use of antibiotics, mechanical debridement, surgery, and removal of the implant.
This article will explore the causes, symptoms, and treatment options for tooth implant infection. We will also discuss how to prevent peri-implantitis from occurring in the first place and provide tips for maintaining good oral hygiene after dental implant surgery. By understanding the risks and taking proactive steps to prevent infection, patients can enjoy dental implants' benefits without worrying about complications.

What Is a Tooth Implant Infection?
A tooth implant infection, also known as peri-implantitis, occurs when bacteria invade the tissues surrounding a dental implant, leading to inflammation and potential damage to the bone supporting the implant. The severity of tooth implant infections can vary from mild gum discomfort to substantial degradation of the teeth and jawbone. If not addressed promptly, a tooth implant infection can cause bone loss and destabilize the implant.
Peri-implantitis can manifest shortly after the implant is restored with a dental crown or even years later. At times, there is little to no pain, so patients may not realize they have an infection.
How Common Is Infection After Dental Implant?
Dental implant infections are relatively rare, with studies estimating the occurrence rate to be around 4-10% of all implant procedures. However, the risk of infection can be higher in patients with certain risk factors, such as poor oral hygiene, smoking, diabetes, and a compromised immune system.
What Can Cause Peri-implantitis?
Several factors can contribute to tooth implant infections, including:
- Poor oral hygiene: Failing to practice good oral hygiene, such as brushing and flossing regularly, can lead to the buildup of plaque and bacteria around the implant, increasing the risk of peri-implantitis;
- Smoking: Smoking has been associated with a higher risk of tooth implant infection due to its negative effects on the healing process and the body's immune response;
- Pre-existing gum disease: Individuals with a history of gum disease (periodontitis) are at a higher risk of developing peri-implantitis, as the bacteria associated with gum disease can also affect the tissues around dental implants;
- Systemic health conditions: Certain systemic health conditions, such as diabetes or autoimmune disorders, can compromise the body's ability to fight off infections and may increase the likelihood of peri-implantitis;
- Poorly fitting prosthetic components: If the crown, bridge, or other prosthetic component attached to the implant does not fit properly, it can create spaces where bacteria can accumulate, leading to tooth inflammation and infection;
- Trauma or excessive force: teeth grinding (bruxism) or improper bite alignment, can damage the surrounding tissues and increase the risk of peri-implantitis;
- Dental cement: Residual dental cement on the implant creates a favorable environment for bacterial growth. This can eventually result in a tooth implant infection, discomfort and potential complications;
- Poor bone quality: If the jaw’s bone has low density, it cannot support the implants and creates a gap between the teeth. Such gaps are home to harmful bacteria.
- Allergic reactions: In rare cases, some individuals may have allergic reactions to the materials used in the implant or prosthetic components, leading to inflammation and tissue damage.

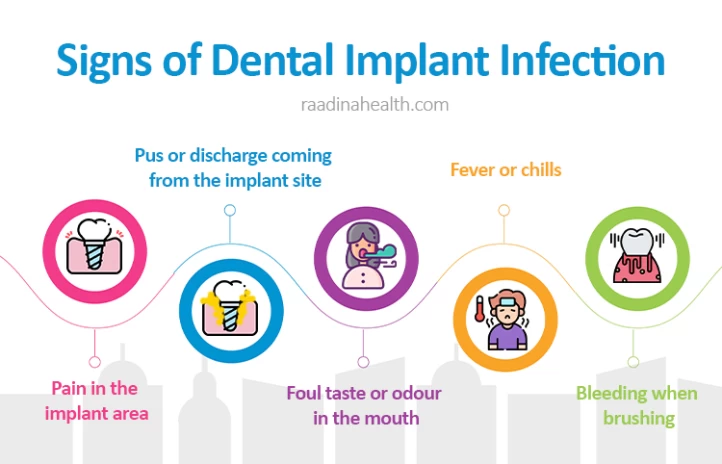
What Are the Signs of an Infected Dental Implant?
Some common tooth implant infection symptoms can include:
- Swollen and red gums around the implant site;
- Pain or tenderness in the implant area;
- Pus or discharge coming from the implant site;
- Foul taste or odour in the mouth;
- Fever or chills;
- Difficulty chewing or biting;
- Loose or wobbly dental implant;
- Gum recession around the implant;
- Persistent bad breath;
- Visible threads on the implant;
- Bleeding when brushing.
How to Diagnose Tooth Implant Infection?
To diagnose a tooth implant infection, a dentist typically thoroughly examines the implant site. This may include taking X-rays to assess the bone and surrounding tissues. A sample of the fluid or tissue around the implant may also be taken for further analysis. Based on the findings of the examination and any additional tests, the dentist will be able to determine if an infection is present and develop a treatment plan accordingly.
How to Treat Tooth Implant Infection?
Common tooth implant infection treatment options are as follows:
Antibiotics
Antibiotics are commonly prescribed to treat post-operative dental implant infections to help control the infection and prevent further complications. The choice of antibiotics and the duration of treatment will depend on the severity of the infection, the type of bacteria involved, and the patient's overall health. Some common antibiotics used to treat dental implant infections are amoxicillin, clindamycin, metronidazole, and ciprofloxacin.
It is essential to take antibiotics exactly as prescribed by your dentist, including completing the full course of treatment even if symptoms improve before the medication is finished. Failure to complete the full course of antibiotics can lead to antibiotic resistance and a recurrence of the tooth implant infection.

Mechanical Cleaning
Mechanical cleaning involves physically removing the bacteria and debris from the infected implant site to help control the infection and promote healing.
Ultrasonic devices and carbon fiber curettes are commonly employed for shallow mucosal pockets. Ultrasonic devices use high-frequency vibrations to break down plaque and bacteria on implant surfaces and pocket walls, while carbon fiber curettes delicately clean shallow pockets without harming the implant. On the other hand, deep pockets may be addressed using gentle scaling instruments or mechanical flossing to ensure thorough cleaning in hard-to-reach areas around the implant. Proper technique is crucial to avoid roughening the implant surface, which could lead to further complications.
On the other hand, deep pockets may be addressed using gentle scaling instruments or mechanical flossing to ensure thorough cleaning in hard-to-reach areas around the implant. Proper technique is crucial to avoid roughening the implant surface, which could lead to further complications.
In certain cases, locally administered antiseptics may be necessary to boost the efficacy of mechanical cleaning. These antiseptics play a crucial role in the treatment process by eradicating any remaining bacteria and preventing future infections. Combining mechanical cleaning techniques with antiseptic treatments can help ensure a successful resolution of dental implant infections while promoting long-term oral health and implant longevity.

Surgery
Surgery may be necessary to treat post-operative dental implant infections that have progressed significantly or are not responding to non-surgical treatments. Surgical intervention aims to remove the infected tissue, clean the implant site thoroughly, and address any underlying issues that may be contributing to the infection.
The surgical treatment for dental implant infection typically involves several steps:
Firstly, an incision is made in the gum tissue surrounding the infected dental implant to access the affected area. This incision allows the dentist to visualize the extent of the infection and plan the appropriate treatment.
Once the area is accessed, the dentist carefully removes the infected implant from the bone and surrounding soft tissues. This removal is crucial to eliminate the source of the infection and allow for thorough cleaning of the area. Debridement, which involves removing any infected tissues, pus, or debris, is then performed to further aid in the healing process.
In cases where the infection has caused bone loss around the implant, bone grafting may be necessary to restore the bone volume and support the implant. This procedure helps stabilize the implant and improves its long-term success;
Antibiotic therapy may be prescribed following surgery to control the infection and prevent its spread.

Implant Removal
Implant removal is usually considered a last resort when all other treatment options have been exhausted. It is performed when the infected dental implants are causing complications such as significant bone loss or damage.
The procedure involves surgically removing the infected implant from the jawbone. This allows the surrounding tissues to heal and the infection to be cleared.
After the implant removal, the area may need to be cleaned and debrided to ensure that all infected tissue is removed. Depending on the severity of the infection, additional treatments such as bone grafting or tissue regeneration may be necessary to restore the health of the jawbone and surrounding tissues.
Dental Implant Infection Home Remedies
It is important to note that treating a dental implant infection at home is not recommended, as infections around dental implants can be serious and may require professional intervention.
However, some dental implant home remedies help manage symptoms and prevent the early dental implant infection from worsening before you can see your dentist. These include:
- Maintain good oral hygiene: Continue to brush your teeth at least twice a day and floss daily, being gentle around the affected area to avoid further irritation;
- Rinse with saltwater: Gently rinse your mouth with warm saltwater (1 teaspoon of salt in a glass of warm water) several times a day to help reduce inflammation and kill bacteria;
- Use a cold compress: Applying a cold compress to the outside of your cheek near the affected area can help reduce swelling and alleviate discomfort;
- Take over-the-counter pain relievers: If you are experiencing pain or discomfort, you can take over-the-counter pain relievers such as ibuprofen or acetaminophen as directed;
- Avoid irritants: Avoid smoking, consuming alcohol, or eating hard or crunchy foods that may irritate the infected area.

How to Prevent Dental Implant Infection?
To avoid an infection after getting dental implants, following proper post-operative care and maintaining good oral hygiene is crucial. Here are some tips to help prevent infections after getting dental implants:
- Take prescribed medications: After your dental implant surgery, your dentist may prescribe antibiotics or pain medication. Take these medications as directed to prevent infection and manage any discomfort.
- Practice good oral hygiene: Brush your teeth gently twice daily and floss daily, being careful around the implant site. Use a soft-bristled toothbrush and non-alcoholic, antimicrobial mouthwash to keep your mouth clean and bacteria-free.
- Avoid touching the surgical site: Do not touch the surgical site with your fingers or tongue to prevent introducing bacteria and causing infection. Follow your dentist's instructions on properly caring for the implant site.
- Follow a soft diet: For the first few days after surgery, stick to a soft diet to avoid putting pressure on the implant site and disrupting the healing process. Avoid hard, crunchy, or sticky foods that may irritate the surgical area.
- Attend follow-up appointments: Schedule and attend all appointments with your dentist to monitor the healing progress of your dental implant. Your dentist will check for signs of infection and provide any necessary treatment.
- Avoid smoking and alcohol: Smoking and excessive alcohol consumption can impair the healing process and increase the risk of infection after dental implant surgery. It is advisable to refrain from smoking and limit alcohol intake during the recovery period.
- Protect your implant: Avoid activities that can put your dental implant at risk, such as chewing on hard objects or participating in contact sports without a mouthguard. Protecting your implant will help prevent damage and reduce the risk of infection.
- Maintain a healthy lifestyle: Eating a balanced diet, staying hydrated, getting enough rest, and managing stress can support your overall health and immune system, promoting faster healing and reducing the risk of infection.
- Use an antimicrobial mouth rinse or warm salt water: It can help eliminate bacteria and lower the risk of dental implant infections.
- Manage bleeding and swelling: To reduce swelling, gently apply ice packs to the area. To control bleeding, gently bite down on clean gauze pads is recommended. It's important to avoid spitting or rinsing excessively, as this can disrupt the natural blood clotting process, which is crucial for healing.
- Limit physical activity: Strenuous exercise should be avoided, as it can prevent excessive blood flow that may hinder the healing process. Your dentist can provide instructions on when it is safe to resume regular exercise routines.

Dental Tourism in Iran
Dental tourism in Iran is rapidly growing as more people look for affordable and high-quality dental care outside of their home countries. Iran is known for having well-trained and experienced dentists, modern dental clinics, and cutting-edge technology as a proper country for dental implants.
Many people travel to Iran for dental procedures such as implants, whitening, veneers, crowns, and orthodontic treatments. The cost of dental treatments in Iran is significantly lower compared to Western countries, making it an attractive option for those seeking affordable dental care.
Additionally, Iran is a popular tourist destination with its rich cultural heritage, historical sites, and beautiful landscapes, making it a desirable location for dental tourists to combine their dental treatment with a vacation.
Frequently Asked Questions About Dental Implant Infection
1) Is taking antibiotics enough to cure dental implant infection?
While antibiotics can be effective in treating dental implant infections, they are not always enough to eliminate the infection. In some cases, dental implant surgery may be required to remove the infected implant.
2) What is the best antibiotic for dental implant infection?
The best antibiotic for a dental implant infection depends on the specific bacteria causing the infection and the patient's medical history and allergies. However, common antibiotics often prescribed for dental implant infections include Amoxicillin, Clindamycin, Augmentationin (a combination of amoxicillin and clavulanic acid), and Metronidazole.
3) Is an implant infection an emergency dentistry problem?
An implant infection is not considered a dental emergency. However, as infections can lead to serious complications if left untreated, it is important to seek professional dental care as soon as possible if you suspect you have one.
4) Can I keep the dental implant if it gets infected?
If a dental implant becomes infected, it is important to seek immediate attention from a dentist or oral surgeon. In some cases, the infection may be treated with antibiotics, and the implant can be salvaged. However, if the infection is severe or the implant becomes loose or fails, it may need removal.
5) Can a dental implant infection go away on its own?
No, a dental implant infection cannot go away on its own. It typically requires prompt treatment by a dentist or oral surgeon to clear up the infection and prevent further complications. Ignoring or neglecting to treat a dental implant infection can lead to more serious issues, such as damage to the surrounding bone and tissues, implant failure, or systemic infection.
6) Can dental implants get infected years later?
Dental implants can potentially become infected years after the initial placement. This can occur as a result of poor oral hygiene, smoking, underlying medical conditions, or trauma to the implant site.
7) How long does a dental implant infection take to heal?
The time it takes for a dental implant infection to heal will vary depending on the severity of the infection and the treatment provided. In some cases, the infection may clear up within a few days with antibiotics, while more severe infections may require longer treatment and possibly implant removal.
8) How long after a dental implant can you get an infection?
Infections after a dental implant procedure are rare but can occur anytime during healing. The risk of infection is highest in the immediate days following the surgery, but it can also develop weeks or even months later.
 WhatsApp
WhatsApp
 Telegram
Telegram
 Facebook
Facebook
 Email
Email


No reviews
Your comment