Testicular Biopsy Procedure: How to Retrieve Sperm for IVF?
Fertility Treatment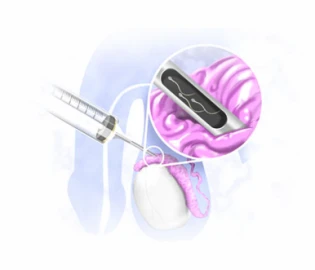
Testicular biopsy is an effective technique for diagnosing the cause of male infertility, cancer tissue or for sperm extraction for IVF in men with azoospermia. In most cases, a biopsy is performed surgically, under local anesthesia, and by the hands of a specialist or a trained health professional. If you have more questions about the procedure, complications, and recovery period of testicular biopsy for infertility, continue reading.
What Is Testicular Biopsy?
A testicular biopsy involves removing a small piece of the testicle to check for sperm production. The process of producing sperm takes place in the seminiferous tubules in the testicles. In the seminiferous tubules, germ cells develop into mature sperms within 64 days and through 16 stages.
By examining the samples obtained from testicular biopsy, the doctor can check the presence or absence of germ cells and sperms and the development of the germ cells. If there is a healthy sperm, it can be extracted and used in IVF and other assisted reproductive techniques.
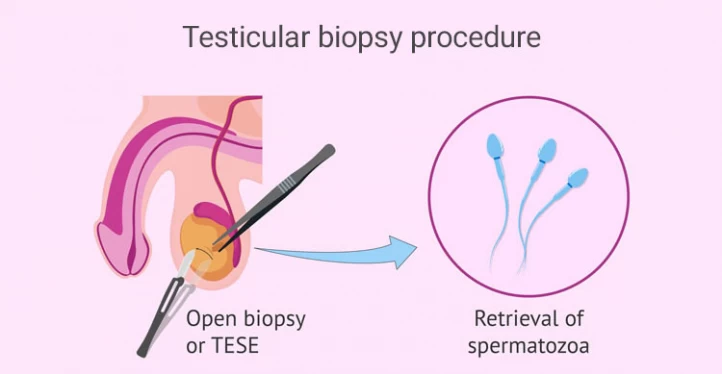
It should be noted that the open testicular biopsy technique is the only way to diagnose the presence or absence of sperm in men with azoospermia. This technique is performed either by surgery (TESE method) or with a special needle (PESA method); in both methods, sperm retrieval is performed under local anesthesia (in most cases) and in a sterile room.

What Can I Expect from a Testicular Biopsy?
In an open testicular biopsy, a small piece of one or both testicles is removed and examined by a urologist or fertility specialist. Usually, the biopsy technique is used to diagnose the cause of infertility in patients with normal FSH levels (Follicle-stimulating Hormone). In these patients, it is not possible to distinguish obstructive azoospermia from spermatogenesis defects or through a spermogram test.
If the testicular biopsy results are normal, the patient does not have testicular cancer, and the organs responsible for producing the sperm are functioning well. However, if the test results are abnormal, it shows that the patient has lumps, azoospermia, or orchitis and needs further treatments.
Although testicular biopsy for sperm retrieval is a simple procedure, you have to expect some side effects, such as pain in the testes, possible bleeding, infection, swelling, discoloration of the scrotum, and discomfort while sleeping.
Testicular Biopsy for Azoospermia
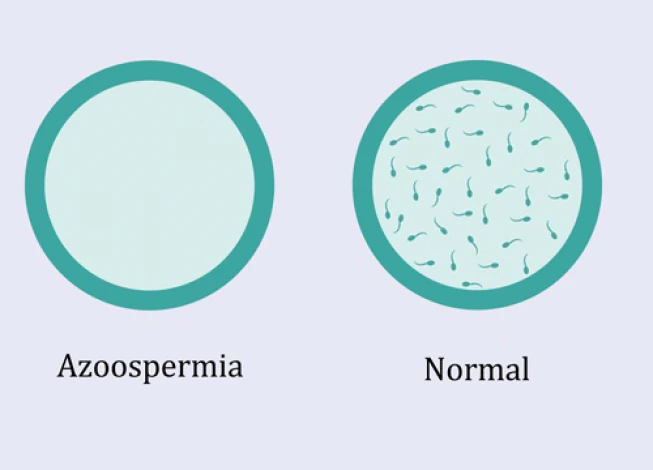
Having no sperm in at least two semen samples is called azoospermia. A blockage causes this problem in ejaculation tracts or when the testes do not produce sperm. Although the only definitive way to diagnose azoospermia is the testicular biopsy, sometimes blood tests, clinical examinations, and genetic tests are used. This procedure directly examines the testicular tissue, providing crucial insights into the root causes of testicular biopsy azoospermia.
For men with azoospermia, a testicular biopsy is done to harvest sperm from their testes for ICSI or IVF use. Of course, when the male partner doesn’t have the bilateral seminal vesicles, performing a biopsy is useless.
It is worth mentioning that in the past, testicular biopsy for azoospermia used to be done on a single part of the testicle. Still, several samples are received from different parts of the testicles because each part of the testicle produces a certain amount of sperm; maybe the doctor can find sperm in one specific part of the testicle.
What is the Testicular Biopsy Procedure?
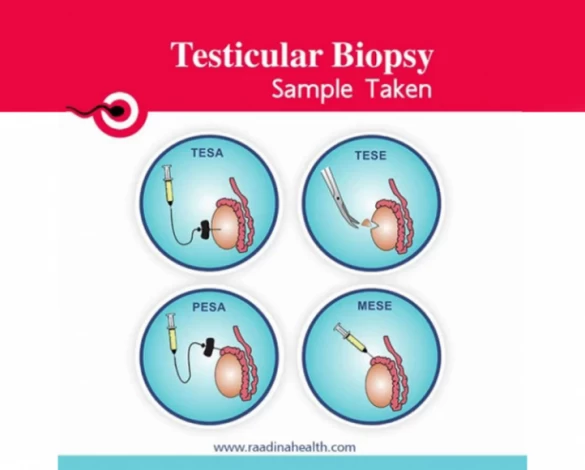
Testicular biopsy for IVF is done in four ways: percutaneous epididymal sperm aspiration (PESA), testicular sperm extraction (TESE), testicular sperm aspiration (TESA), and microsurgical epididymal sperm aspiration (MESA). Usually, the surgeon uses an ultrasound probe or MRI/X-ray scanning to guide the surgical tube correctly.
In the following, all these methods are introduced in detail:
Percutaneous Epididymal Sperm Aspiration (PESA)
The PESA technique is used in cases where the patient has obstructive azoospermia; it means that although his testicles produce sperm, the sperm cannot enter the semen due to congenital disabilities, damage to the tubes that carry sperm, and infection.
Before doing PESA, the doctor advises you to shave your genital hair and attend the surgery center on an empty stomach in the morning. After sterilizing the room and administering local anesthesia, the sperms are extracted from the epididymis (inner tube of the testicle) with a syringe and insulin needle. Then, the sperm sample is delivered to the laboratory for further examination.
If the test is positive, the person can be a candidate for microinjection, but if no sperm found in the testicular biopsy, the patient should be surgically treated. The doctors advise this method to reduce the costs and avoid testicular sampling.
Testicular Sperm Extraction (TESE)
In TESE, the patient should shave off his genital hair and attend the surgery center on an empty stomach in the morning. A caregiver is usually needed for TESE because this surgery is invasive. In this method, the surgery room is also sterilized, and local anesthesia is administered; however, injecting intravenous sedatives at the doctor's discretion and the patient's request is possible.
The appropriate drug should be injected into the spermatic cord (blood vessels connecting the testicles to the abdominal cavity), and the incision placed to anesthetize the patient.
After examining the testis's tissue under laboratory microscopes, if sperm is observed, the microinjection method can be used to treat the infertile man.
What to Do If No Sperm Found in TESE?
If no sperm is found in the testicular biopsy, the doctor must repeat the biopsy to ensure the patient has azoospermia. This meticulous approach becomes particularly crucial in cases where no sperm is found after TESE (Micro TESE method), providing an accurate diagnosis and guiding the appropriate course of action for fertility treatment.
Testicular Sperm Aspiration (TESA)
In the TESA method, a less invasive procedure done under local anesthesia, a sample of testicular fluid and tissue is obtained with the help of a special needle. In fact, during the TESA operation, the sperms are gently pulled out by making an incision in the scrotum’s skin. Then, the sperm needed for IVF or ICSI is retrieved from testicular fluid and tissue in the laboratory. This technique is also used for diagnosing azoospermia.
Microsurgical Epididymal Sperm Aspiration (MESA)
The MESA method is used when the patient suffers from epididymis obstruction caused by vasectomy or congenital bilateral absence of the vas deferens. After carefully observing the epididymal tubes under the microscope, the doctor extracts healthy and motile sperm and uses them in IVF or ICSI. The doctor may also freeze some high-quality sperm for future use.
Why Is Testicular Biopsy Done?
Testicular biopsy is used to diagnose sperm problems such as insufficiencies and diseases; also, it is helpful to retrieve sperm from the testicle to be used in IVF and other fertility treatment techniques such as IUI and ICSI.
Of course, it’s worth mentioning that not all azoospermic patients need a biopsy test. Doctors will not take the biopsy test if the azoospermia is due to the lack of seminal vesicles on both sides. Since sperm production differs in various parts of the testicle, a biopsy is done at different points. Today, four parts are considered for the testicle, aand a testis biopsy is done on each part.
After testicular biopsy for IVF, if healthy sperm is collected, the samples are frozen for later use. The sperms are frozen because, in some cases, these samples are the only sperm left for the patient, and the doctor may be unable to find mature sperms in subsequent biopsies.

Best Candidates for Testicular Biopsy
The best candidates for testicular biopsy are those who have very few sperm in their semen analysis, and the following factors cause their sperm problem:
- Congenital lack or blockage of the vas deferens;
- Hormonal problems;
- Radiation exposure, especially in patients with cancer;
- Genetic factors and the formation of sperm-producing genes on the Y chromosome;
- Infectious diseases such as mumps;
- Some drugs, especially the ones used in cancer treatment, etc.
Preparation for a Testicular Biopsy
Before doing a testicular biopsy for sperm retrieval, the patient should take care of himself and inform the doctor about the following points:
- Any bleeding;
- Having an allergy to any drug, including anesthetics and
- The medications he takes.
Also, the patient must shave the hair on the scrotum, around the penis, and groin the night before surgery.
Usually, a biopsy is done under local anesthesia. Still, if it has to be done under general anesthesia at the doctor's discretion, the patient should avoid eating and drinking before the surgery.
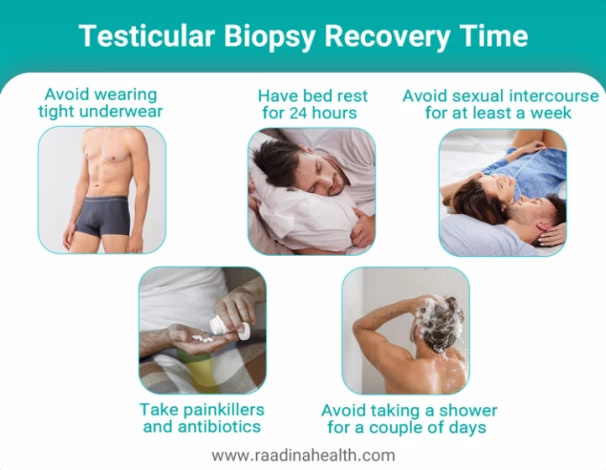
Testicular Biopsy Recovery Time
Although testicular biopsy is not painful, you must follow some postoperative instructions during recovery to minimize discomfort and complications. It is worth mentioning that swelling, mild pain, and light bleeding are common side effects of this procedure, so you don’t have to worry about them.
Here are the things to do after a testicular biopsy:
- Avoid wearing tight underwear;
- Take painkillers and antibiotics;
- Have bed rest for 24 hours;
- Avoid sexual intercourse for at least a week;
- Wear an athletic supporter to protect the testicles from pressure and damage;
- Keep the treated area dry;
- Avoid taking a shower or washing testes for a couple of days;
- Avoid taking blood thinners such as aspirin for a week;
- In case of having pain, take prescribed painkillers or acetaminophen;
Is Testicular Biopsy Painful?
Typically, testicular biopsy for male infertility is less painful than done under general or local anesthesia. However, some patients who have undergone this procedure assert that they felt mild pain and pressure in their scrotum during the operation and a couple of days after, but the discomfort was eliminated very soon.
Testicular Biopsy Side Effects
A testicular biopsy for IVF is a simple operation, and the person will not have severe bleeding or infection; mild pain and swelling are perfectly normal. Some people are worried about the aggravation of fertility problems after the operation. We should note that this operation will not affect the erection or heighten infertility, so the patients should not be worried.
If you observe the following problems after testicular biopsy, contact your doctor:
- Severe pain;
- Extreme swelling;
- Fever above 38 degrees; and
- Severe bleeding.
The Timing of Surgical Sperm Retrieval for IVF
Whether retrieving sperm before or during the IVF treatment is a hard decision you and your partner should take; if you undergo sperm retrieval before the start of the IVF procedure, you need to pay extra money to freeze the sperm. Still, you will have plenty of time to decide whether to continue the fertility treatment.
On the other hand, embryologists usually recommend that surgical sperm retrieval be performed on the day of egg retrieval because the egg is fresh and of higher quality. So, if you are decisive about continuing the IVF treatment, it is suggested to undergo testicular biopsy when your partner’s egg is harvested.
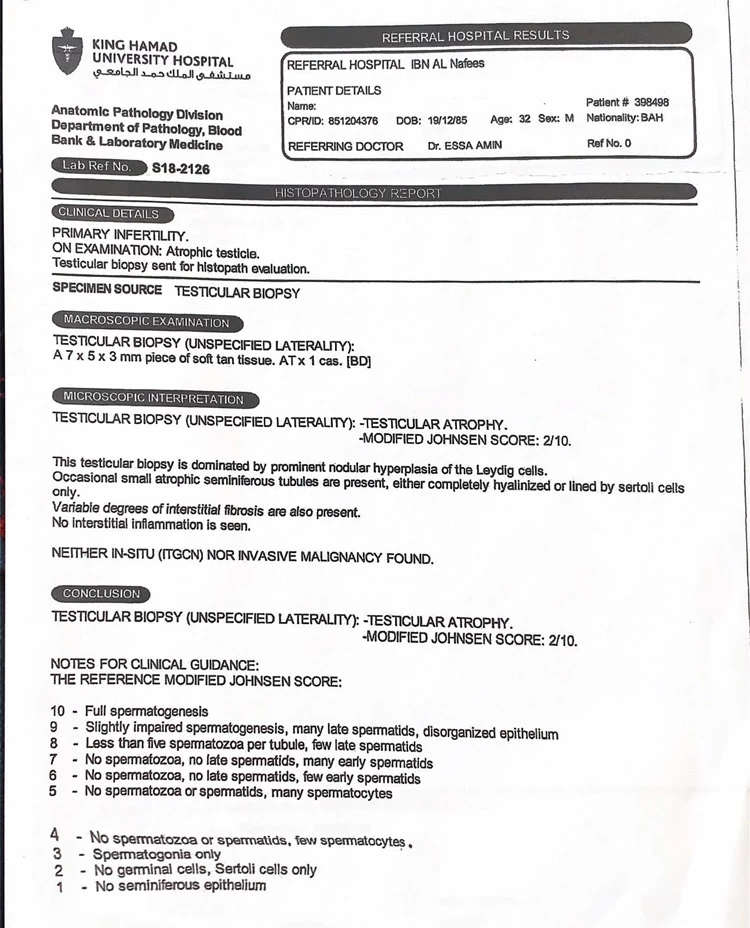
Testicular Biopsy Results
Interpreting the results of the testicular biopsy for IVF is very important in choosing the best treatment. Although testicular biopsy is a simple operation performed only through a small incision in the skin of the scrotum, interpreting its results is essential and difficult. In the fertility center, a pathologist examines the samples. In some cases, the patient is infertile and does not have any germ cells. In this situation, the doctor recommends using a donated embryo for the patient.
In some patients, the germ cells have evolved in several stages, but at a particular stage, this evolution has stopped. This group also does not have sperm in their semen, but their situation differs from those without germ cells. Because these people can get better by using particular medicines, and the developmental stage of their germ cells can be completed, or in some cases, their immature sperms can mature in the laboratory. It is worth mentioning that both of these groups suffer from azoospermia.
Interpretation of Testicular Biopsy’s Result
In general, the interpretation of testicular biopsy results is divided into four categories:
- Natural: in these cases, testicular problems are not the cause of the lack of sperm.
- Stop in sperm evolution: sperm must go through 16 stages to evolve. Sometimes, this evolution stops at one point.
- Insufficient sperm production: in this case, the complete development of sperm occurs in some parts of the testicle, but these parts are so limited that the sperm does not appear in the semen.
- Lack of germ cells: these patients do not have germ cells in their testicles.
Sometimes the biopsy test shows that the testicle has its normal function. The lack of sperm in the testicle relates to obstructive azoospermia (OA), which results from a blockage of the male reproductive tract.
Concluding Remarks and Recommendations
Regarding the abovementioned points, it seems that today, the best way to diagnose a variety of sperm problems (including low count, low quality, low motility, improper shape, etc.) is a testicular biopsy. In addition to its diagnostic use, it provides the basis for using the most appropriate methods to treat male fertility problems.
Therefore, it is urgent to increase the awareness of infertile couples about this operation when they refer to fertility centers and consult a specialist doctor.
FAQs about Testicular Biopsy
Can Testicular Biopsy Diagnose Cancer?
Testicular biopsy is mainly used to diagnose the cause of male infertility or to retrieve sperm from the testicles. Basically, this method is not used to diagnose testicular cancer as it can trigger cancerous cells and increase the chance of cancer spreading. Usually, other methods, such as radical inguinal orchiectomy or ultrasound tests, are used to detect testicular cancer.
Should I take other tests along with a testicular biopsy?
Suppose the results of the spermogram show that you have azoospermia or oligozoospermia. In that case, you must take a hormone test and undergo a physical examination to detect the cause.
What is the difference between microsurgical and open testicular biopsy?
In a microsurgical testicular biopsy, more sperms are retrieved, and less damage is done to the testicular tissue. On the other hand, an open or conventional biopsy is more invasive and is more suitable for detecting testicular cancer.
What are the disadvantages of surgical sperm retrieval?
Surgical sperm retrieval has limitations and disadvantages, making it less desirable to some fertility specialists and patients. First, it is invasive and involves anesthesia and scarring. Second, it only provides information on the biopsied area, not all parts of the testes. And finally, the results of this test can be interpreted differently, so sometimes, it cannot help the azoospermic patient.
How many testicular biopsies should be done to find sperm?
Usually, the doctor can find healthy sperm in the first four testicular biopsies, but there is no actual limit to the number of times this test can be repeated.
What is a testicular biopsy in male infertility?
A testicular biopsy is a procedure used to examine testicular tissue and retrieve sperm in men dealing with infertility. It helps determine whether the testes are producing sperm and whether sperm can be collected for IVF or ICSI.
What is testicular biopsy for azoospermia?
In men with azoospermia, a testicular biopsy helps identify whether sperm production exists inside the testes. If sperm are found, they can be retrieved directly from the tissue and used for IVF or ICSI.
What is the success rate of a testicular biopsy?
The success rate depends on whether sperm production is present. In obstructive azoospermia, sperm retrieval rates are often 90–100%, while in non-obstructive azoospermia, success rates typically range from 30–60%, depending on the underlying cause.
What is the recovery time after a testicular biopsy?
Most men recover within 3–5 days, although mild swelling or discomfort can last up to a week. Full healing of the tissue usually takes about 2 weeks.
What does it mean if no sperm are found in a testicular biopsy?
When no sperm are found, it usually indicates severe non-obstructive azoospermia or impaired sperm production. Further evaluation—including hormone testing and genetic screening—may be needed to determine the next steps.


 WhatsApp
WhatsApp
 Telegram
Telegram
 Facebook
Facebook
 Email
Email










User
-Thank you for the article. It really brings to light what we should know about testicular biopsy. I have two questions: 1. What are the "four" sites of preferred TESE? 2. Correction: you mentioned in the third FAQ that open biopsy is the preferred method for detecting testicular cancer! This was refuted earlier. Could that be a mistake or do you stand by that? Dr Njuma, Urologist