Vasectomy Procedure: Recovery, Side effects & Effectiveness
Fertility Treatment
A vasectomy procedure is a permanent form of contraception in men that involves cutting or blocking the tubes that carry sperm from the testicles to the penis. Most vasectomies can be reversed. However, the success rate of vasovasostomy varies and is not guaranteed. Vasectomy reversal can be tried even if several years have passed since the original procedure — but the longer it has been, the less likely it is that the reversal will be effective.
In this article, we explore the vasectomy (blocking or cutting vas deferens tube) procedure, vasectomy recovery, and its potential side effects.
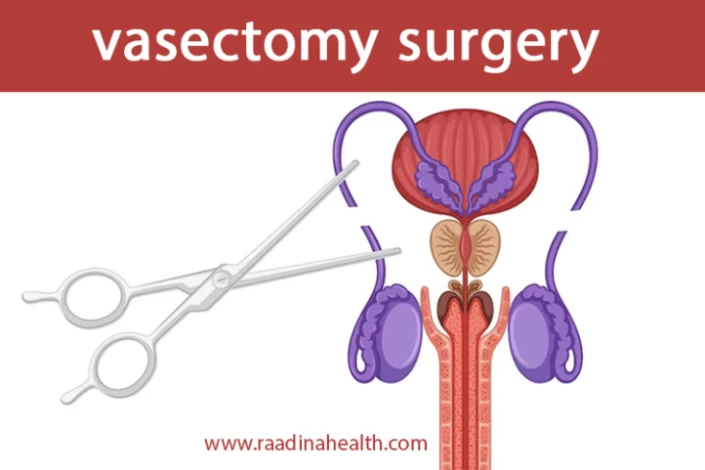
What is a Vasectomy?
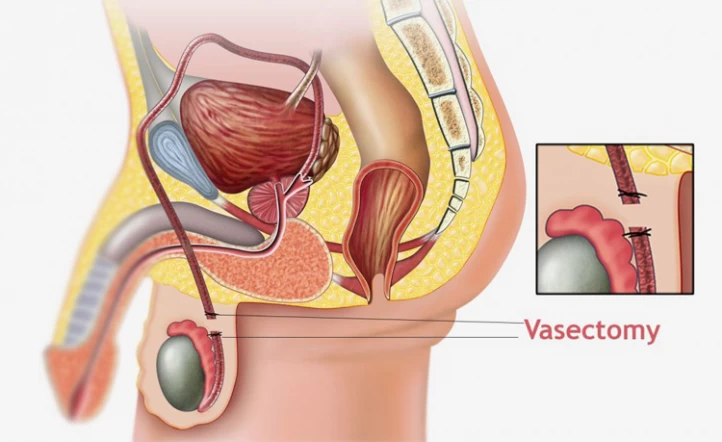
Vasectomy is the best option for men who want a permanent form of birth control. During this surgical procedure, the doctor will make a small incision in the scrotum and cut or block the vas deferens. It is a safe and effective procedure that can be done in a doctor's office. The vasectomy procedure is typically done under local anesthesia and takes less than 20 minutes. It is important to note that vasectomy only prevents sperm from being released during ejaculation and, therefore, makes a man unable to father children and does not affect male sexual desire or ability to ejaculate.
What Is The Vasectomy Procedure?
Understanding the different techniques involved in the vasectomy procedure is crucial for those considering this form of birth control. Below, we'll explore the conventional and innovative approaches of no-scalpel vasectomy, highlighting their respective methods and differences.
Conventional Vasectomy:
Conventional vasectomy is a surgical procedure involving one or two small incisions made in the skin of the scrotum to access and cut the vas deferens, the tubes responsible for carrying sperm from the testicles to the urethra. During the procedure, the surgeon removes both ends of the vas deferens and ties them at two points, typically 1 cm apart, using silk thread. Once the vas deferens are severed or blocked, they are returned to their original position, and the incisions are closed using sutures or surgical glue.
No-Scalpel Vasectomy:
No-scalpel vasectomy is a minimally invasive alternative to conventional vasectomy. This technique involves using a small, sharp instrument to puncture the skin of the scrotum and locate the vas deferens without making any incisions. Once the vas deferens are located, the surgeon places a small clip or clamp on their ends to block sperm flow. Unlike conventional vasectomy, which requires stitches to close the incisions, no-scalpel vasectomy may not necessitate stitches as the puncture site can heal independently or be sealed with surgical glue. It's important to clarify that no-scalpel vasectomy does not involve the use of a laser to cut and seal the vas deferens, as some may mistakenly believe.
Both conventional and no-scalpel vasectomy procedures provide effective methods of permanent contraception, but they differ in their approach and techniques used during the surgery. Each technique has its advantages, and individuals considering a vasectomy should discuss their options with a healthcare provider to determine the most suitable approach for their needs.
Contact us for a free initial consultation about Vasectomy surgery.
WhatsAppTelegramFacebookEmailWhat are Vasectomy Aftercare Instructions?
After a vasectomy, it is important to follow the aftercare instructions provided by the surgeon to promote the healing process and reduce possible complications.
Vasectomy recovery tips may include:
- Remove the dressings after 24 hours and place 1-2 sterile gauze pads on the surgical site;
- Wear supportive underwear or scrotal support for a week after the surgery to provide comfort and support;
- Avoid taking a bath or using a hot tub for 24 hours after the vasectomy;
- Dry the incision site immediately after taking a bath to prevent infection;
- Refrain from sexual activity and ejaculation for one week to prevent severe pain and discomfort during ejaculation;
- Rest and avoid strenuous activities for a week to allow the incision site to heal;
- Apply ice packs to the scrotum the night of the vasectomy and the following day for 20 minutes at a time;
- Take over-the-counter pain medication as directed by the surgeon to manage any discomfort.
How Does Vasectomy Prevent Pregnancy?
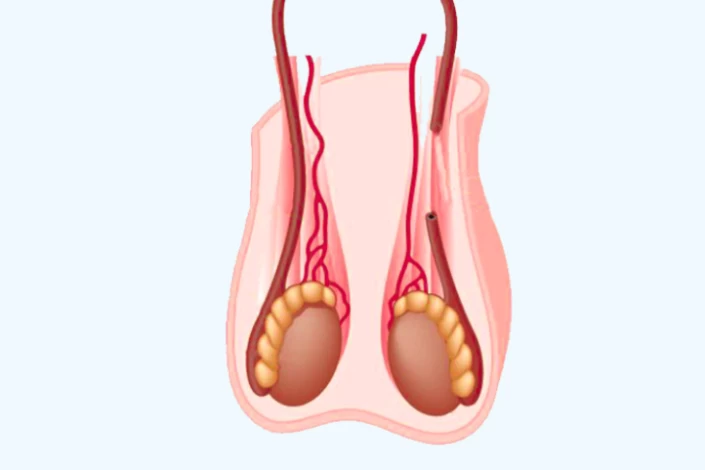
Vasectomy can prevent pregnancy by cutting or blocking the vas deferens, which are the tubes that carry sperm from the testicles to the urethra. As a result, the man's semen will no longer contain sperm, and therefore, pregnancy cannot occur.
However, it is important to confirm that the procedure was successful and that the man's semen no longer contains sperm After a vasectomy. This is typically done through follow-up tests, which may include a physical examination of the incision site about a week after the blockage of the vas deferens and a semen analysis (to examine azoospermia) at least three months after the vasectomy. Additionally, a post-vasectomy sperm count is done four months after the surgery (one month after the first test) to confirm that the vasectomy was definitively successful.
What is the Success Rate of Vasectomy?
"How effective is a vasectomy?" is a question often posed by individuals considering permanent contraception. Research indicates that vasectomy effectiveness is evident, with approximately 15 to 20 pregnancies per 10,000 populations, indicating its high success rate in preventing conception. However, it's important to note that a vasectomy does not provide immediate protection against pregnancy, and 20% of patients may still have sperm in their semen for at least three months after the surgery. Therefore, couples should use an alternative form of birth control until a follow-up test confirms that there are no sperm present in the semen.

How to Verify the Success of My Vasectomy?
Typically, around 12 weeks post-procedure, you'll be asked to provide a semen sample for analysis to check for the presence of sperm. Once the tests ascertain that your semen is devoid of sperm, your vasectomy is deemed successful, and you can discontinue the use of additional contraception. Some individuals may require two tests for confirmation. However, until it's confirmed that your semen is sperm-free, it's advisable to continue using another form of contraception. In rare instances, a few men may retain minimal quantities of immobile sperm in their system, which pose a lower risk of impregnation. If you fall into this category, your doctor will discuss available options with you. Furthermore, the testing process assists in identifying exceedingly rare occurrences, such as the spontaneous reconnection of the vas deferens tubes.
What are the Risks and complications of Vasectomy Surgery?
Vasectomy is a safe and simple form of permanent birth control for men as it does not affect factors such as testosterone production, orgasm occurrence, or sex drive level.
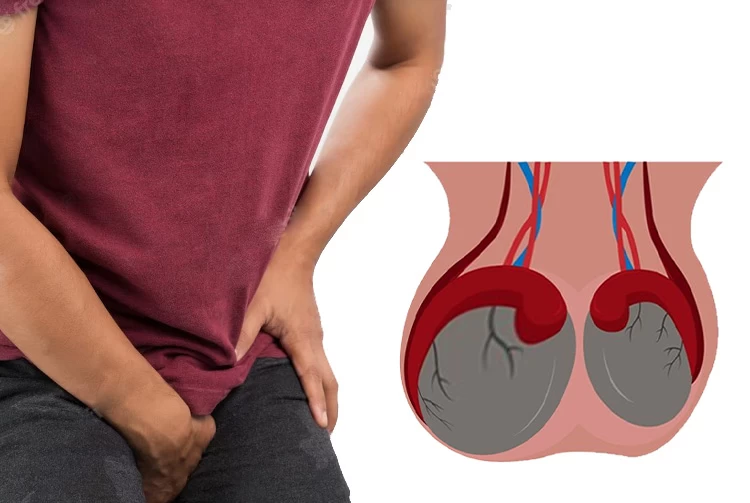
The most common complications of vasectomy are swelling, bruising, inflammation, and infection. Although these complications are often mild, they should be reported to the doctor.

How Soon Can Patients Resume Sex Post-Vasectomy?
Patients are typically advised to wait at least a week after a vasectomy before engaging in sexual activity. This allows time for the incision site to heal and reduces the risk of pain and damage to the testicles. After the initial week, patients should still use contraception during sexual activity until they have confirmed with their doctor that their semen is free of sperm. This typically requires two post-vasectomy semen analyses. The first sperm analysis test is usually performed after ten ejaculations after the surgery. Once the patient has received confirmation that their semen is sperm-free, they can resume sexual activity without the need for additional contraception.
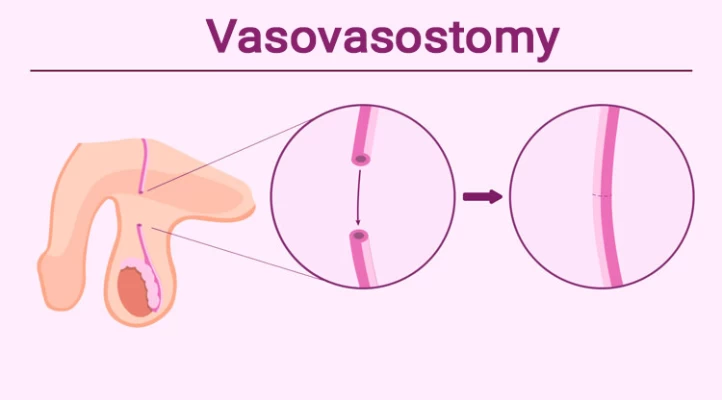
Side Effects of Vasovasostomy
As mentioned, men may choose to have a vasovasostomy to allow them to father children again, which is a surgical procedure to reconnect the vas deferens and reverse the effects of a vasectomy. During a vasovasostomy, the surgeon makes small incisions in the scrotum to access the vas deferens. A sample of the semen in the testicles is then removed to be checked for the presence of healthy and mature sperm.
Next, the place where the vas deferens were cut is reconnected. If not possible, the ends of the vas deferens are connected to the part of the testicles containing mature sperm.
It should be noted that the surgery may come with the same side effects as vasectomy. Additionally, it can take at least 1 to 3 weeks for fertility to return in most cases.
Who are Good Candidates for Vasectomy?
Vasectomy is not suitable for all men as it completely prevents pregnancy, and its reversal surgery is relatively complicated.
Good candidates for vasectomy are men who are over 40 and have two or more children. It is a permanent form of birth control and should only be considered if a man is certain he does not want to have any more children or does not want to have any children at all. Research indicates that men who undergo a vasectomy at a young age and have either no children or only one child are more likely to experience regret compared to those who undergo the procedure at an older age.
Vasovasostomy is a surgical procedure that is performed to reverse a vasectomy. It is done in the operating room under general anesthesia or spinal anesthesia with an operating microscope. Vasovasostomy takes up to 2 hours, and its success rate is not 100%.
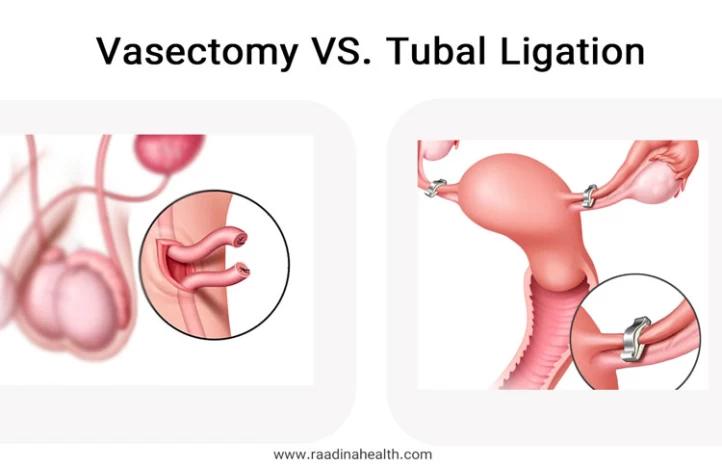
Vasectomy vs Tubal Ligation: Which is a Better Option?
Both vasectomy and tubal Ligation procedures are highly effective in preventing pregnancy with very high success rates. However, vasectomy is a less invasive procedure that can be done in an outpatient setting with local anesthesia. It has a shorter recovery time and fewer complications compared to tubal ligation. Also, the cost of vasectomy surgery is lower, and there is no risk of ectopic pregnancy.
Is It Possible to Have a Baby After Vasectomy Surgery?
Frozen Sperm
If you've undergone a vasectomy and find yourself regretting the decision or hoping to expand your family, rest assured, there are methods available for conceiving even after the procedure. Many individuals experience a change of heart regarding vasectomy, and advancements in reproductive technology offer avenues for conception post-vasectomy. Whether through the use of frozen sperm, vasectomy reversal surgery, or assisted reproductive techniques like in vitro fertilization (IVF), there are paths forward for those seeking to become parents again.
Getting pregnant with frozen sperm after undergoing a vasectomy involves several steps. Firstly, the individual who has undergone a vasectomy must visit a fertility clinic to discuss their options. The clinic will then extract and freeze sperm before the vasectomy procedure. Once the decision to conceive is made, the frozen sperm is thawed and prepared for insemination or in vitro fertilization (IVF). Insemination involves inserting the sperm into the uterus during ovulation, while IVF involves fertilizing eggs outside the body and then implanting the embryo into the uterus. The success of conception depends on various factors such as sperm quality, the woman's reproductive health, and the chosen method of conception. Therefore, it's crucial to consult with fertility experts to determine the most suitable approach for achieving pregnancy.
Testicular Biopsy
While a testicular biopsy and a vasectomy are two distinct procedures, they can be related in the context of male reproductive health. A testicular biopsy may be performed to assess fertility potential or to diagnose conditions affecting the testicles, such as testicular cancer. In cases where a man is considering a vasectomy, a testicular biopsy may be recommended as part of the pre-procedure evaluation to ensure there are no underlying issues that could affect the success or outcome of the vasectomy. Additionally, in situations where a vasectomy reversal is being considered, the results of a testicular biopsy may provide valuable information about the fertility potential and the likelihood of successful reversal. Therefore, while the procedures serve different purposes, a testicular biopsy can be relevant in the broader context of vasectomy decision-making and fertility management.
Final Word
Vasectomy is a permanent and irreversible method of contraception for men. While it is highly effective and causes no serious complications, individuals must carefully consider the long-term implications of such a decision. With advancements in contraceptive methods, there are many other options available that are reversible and provide more flexibility for individuals who may change their minds in the future. It is recommended that individuals explore all their options and consider their long-term reproductive goals before opting for a permanent method like vasectomy.
Frequently Asked Questions on Vasectomy
1) What is the success rate of vasectomy reversal?
The success rate of vasectomy reversal can vary depending on factors such as the patient's age, the length of time since the vasectomy, and the presence or absence of other male infertility problems. Generally, the success rate of vasectomy reversal is around 40-90%, with the highest success rates seen in men who have had the vasectomy less than ten years ago. It is important for men considering vasectomy reversal to consult with a qualified urologist to discuss their specific situation and the potential success rate of the procedure.
2) How effective is a vasectomy in preventing pregnancy?
Vasectomy is one of the most effective forms of contraception available, with a success rate of over 99%. However, it's crucial to understand that the effectiveness of a vasectomy is not immediate. After the procedure, sperm can still be present in the semen, so it's essential to use alternative birth control methods until a post-vasectomy semen analysis confirms the absence of sperm. Once this analysis confirms sterility, a vasectomy is considered a highly reliable method of preventing pregnancy.
3) Is a vasectomy reversible?
While vasectomy reversal is technically possible, it's important to note that it's not always successful. The success of a vasectomy reversal depends on various factors, including the length of time since the vasectomy, the technique used during the original procedure, and individual factors such as age and fertility. Success rates for vasectomy reversals can vary widely, ranging from around 40% to 90%. Additionally, the procedure itself is more complex and invasive than a vasectomy, and it may not always restore fertility to pre-vasectomy levels.
4) What are the risks associated with a vasectomy?
Like any surgical procedure, a vasectomy carries some risks, although they are relatively low. Potential risks include infection, bleeding, hematoma (blood collection outside a blood vessel), and forming a small lump or cyst in the scrotum. In very rare cases, some men may experience chronic pain or discomfort in the testicles or pelvic region after a vasectomy, a condition known as post-vasectomy pain syndrome (PVPS). However, the vast majority of men who undergo vasectomy experience minimal complications and a quick recovery.
5) How long does it take to recover from a vasectomy?
Recovery time after a vasectomy can vary from person to person. Still, most men can expect to resume their normal activities within a few days to a week after the procedure. It's common to experience some discomfort, swelling, and bruising in the scrotal area immediately following the vasectomy, but these symptoms typically subside within a week or two. During the recovery period, it's advisable to avoid strenuous activities, heavy lifting, and sexual intercourse until any discomfort has resolved.
6) Will a vasectomy affect my sexual function or libido?
No, a vasectomy does not affect sexual function or libido. The primary purpose of a vasectomy is to prevent sperm from being ejaculated during orgasm. Still, it does not alter the production of testosterone or other hormones involved in sexual desire and performance. Men who have undergone a vasectomy can still achieve erections, ejaculate normally, and experience orgasms just as they did before the procedure.
7) Can a vasectomy increase the risk of prostate cancer?
There is no evidence to suggest that vasectomy increases the risk of prostate cancer. Numerous studies have been conducted to investigate the potential link between vasectomy and prostate cancer risk, and the overwhelming majority of research has found no association between the two. The American Urological Association and other medical organizations have stated that there is no credible evidence to support the idea that vasectomy contributes to an increased risk of prostate cancer.
8) Is there an age limit for getting a vasectomy?
While there is no strict age limit for undergoing a vasectomy, most healthcare providers recommend the procedure for men who have completed their family or who are certain they do not want to have children in the future. It's important for individuals considering a vasectomy to carefully consider their decision, as the procedure is intended to be permanent. Some healthcare providers may also require individuals to be of a certain age or maturity level before performing a vasectomy to ensure that the decision is informed and voluntary.
9) Will a vasectomy affect hormone levels or masculinity?
No, a vasectomy does not affect hormone levels or masculinity. The procedure only interrupts the flow of sperm from the testicles to the urethra; it does not alter the production of testosterone or other hormones involved in masculine characteristics. Men who have undergone a vasectomy will continue to produce testosterone at the same levels as before the procedure, and they will not experience any changes in their physical appearance, sexual functioning, or overall sense of masculinity.
10) What Happens to Sperm After Vasectomy?
After a vasectomy, sperm production in the testicles continues as normal. However, since the vas deferens, the tubes that carry sperm from the testicles to the urethra, are severed or blocked during the procedure, sperm cannot pass through. As a result, the body reabsorbs the sperm, recognizing them as foreign particles. This process, known as sperm resorption, gradually breaks down and eliminates the sperm. While some sperm may remain in the reproductive system immediately after the vasectomy, they are typically cleared over time. This natural process does not affect sexual function or the production of semen.
11) How long does a vasectomy take?
The duration of a vasectomy procedure typically ranges from 20 to 30 minutes. However, the exact time may vary depending on the surgeon's experience, technique, and individual anatomy. Patients are usually able to return home shortly after the procedure and resume normal activities within a few days.














No reviews
Your comment