Sperm Extraction with Micro-TESE: How Does It Work?
Fertility Treatment
Microscopic testicular sperm extraction (microTESE) stands at the forefront of male infertility treatment, offering a beacon of hope to couples grappling with male factor infertility, notably non-obstructive azoospermia. This state-of-the-art procedure represents a paradigm shift in assisted reproductive technologies, presenting a pathway for couples to realize their dreams of parenthood through innovative methods like IVF.
The microTESE procedure employs sophisticated surgical microscopes to meticulously identify and extract small sperm clusters directly from the testicles. Unlike conventional sperm retrieval methods such as testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA), microsurgical sperm collection through microTESE precisely targets specific areas within the testicular tissue where sperm are most likely to be found, enhancing the chances of successful extraction.
In instances where no sperm are detected following a TESE procedure, the prospects of conceiving a biological child may seem daunting. However, microTESE offers a ray of hope by delving deeper into the testicular tissue to locate viable sperm, thus expanding the possibilities for fertility treatment success.
This article delves into the nuances of microTESE recovery and its associated benefits and side effects. It illuminates its success rates and offers insights into its transformative impact on male infertility treatment.

What Is a Micro-tese (Microscopic Testicular Sperm Extraction)?
Micro-TESE, or Microscopic Testicular Sperm Extraction, is a surgical procedure used to retrieve sperm from the testicles of men with non-obstructive azoospermia (NOA). This procedure is performed under a microscope, allowing the surgeon to identify and extract small amounts of sperm from the testicular tissue. The sperm is then used for assisted reproductive techniques such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) to help a couple conceive.
Micro-TESE surgery is considered to be a more advanced and effective technique for retrieving sperm compared to traditional TESE, as it allows for a more precise and targeted extraction of sperm, increasing the chances of finding viable sperm for use in assisted reproductive technologies such as IVF.
How Does Micro-TESE Procedure Done?
As previously noted, micro-TESE is a valuable option for men with NOA-related infertility who are hoping to conceive with their wife or partner. The procedure unfolds as follows:
Step 1: Anesthesia and Incision
The patient is usually put under general anesthesia for the microscopic testicular sperm extraction (micro-TESE procedure). To reach the testicles, the surgeon then makes a tiny incision in the scrotum, about 1 to 2 cm.
Step 2: Microscopic Examination
To find dilated seminiferous tubules that most likely contain sperm, the surgeon carefully inspects the testicular tissue under a powerful microscope (up to 20x magnification). After that, these regions are taken out and sent to a lab to check for sperm.
Step 3: Extraction of Sperm
In order to extract viable sperm, the surgeon keeps examining every part of the testicular tissue. The incision is closed after the sperm collection, and the patient is given time to recuperate from the anesthesia.
Step 4: Sperm Freezing
For use in assisted reproductive procedures like intracytoplasmic sperm injection or in vitro fertilization (IVF), the extracted sperm will be frozen. Thankfully, sperm cells are not adversely affected by the freezing process.
One benefit of Micro-TESE is that it eliminates the need for repeat sampling for individuals who need IVF treatment. It is also utilized for fertilization using the ICSI treatment of microinjection.

What Preparations Must Be Done Before Micro-TESE?
The patient must take precautions and prepare for the procedure before undergoing the micro-TESE, including the following:
- Remove extra hair from the surgical site, such as the scrotum;
- Shave the area surrounding the penis and groin the night before the procedure;
- Consult your doctor in case you are using any kind of anticoagulants, such as aspirin, warfarin, ibuprofen, or nonsteroidal anti-inflammatory medicines;
- Notify your surgeon whether you have an allergy or intolerance to any anesthetic medications;
- Report any bleeding to your urological surgeon.
Micro-TESE Aftercare
Patients will be monitored in a recovery area to ensure they are stable and recovering well from the surgery after the procedure. They may experience some discomfort or pain, which can be managed with pain medication prescribed by the surgeon.
Patients will also receive post-operative instructions from the surgeon to ensure a smooth recovery from Micro-TESE.
·Consistently take Tylenol, ibuprofen, antibiotics, and pain relievers as directed;
·To support the scrotum and reduce swelling, wear a tight pair of jockey shorts for a week.
·For the first 48 hours, apply ice packs to the scrotum for 15 minutes every hour to reduce swelling;
·Refrain from wearing restrictive or absorbent clothing around the surgical site;
·Avoid strenuous activities for the first five days following the procedure;
·Steer clear of aspirin products for two weeks;
·Avoid running, heavy lifting, long walks, cycling, and straining for one to two weeks following Micro-TESE surgery;
·Avoid swimming for two weeks;
·Prevent sexual activity for two weeks;
·And notify your doctor of any severe swelling, inflammation, bleeding, or redness at the surgical site.
Differences Between Biopsy and Micro-TESE
The biopsy approach involves removing and examining only a small section of the testicle. The sampling method in testicular biopsy is considered one of its defects, as the unstudied areas might have the capacity to produce sperm. On the other hand, in micro-TESE, as soon as sperm is discovered, it can fertilize an egg or be preserved for use later.
What Is the Difference Between TESE and Micro TESE Infertility Treatment?
Men with obstructive azoospermia typically undergo one of two surgical procedures called testicular sperm extraction (TESE) or microscopic testicular sperm extraction (micro-TESE). These 2 methods involve separate surgical techniques.
Testicular Sperm Extraction (TESE) Surgery, a common procedure involves making a small incision on the testicle skin and extracting tiny pieces of testicular tissue for examination. Nevertheless, the micro-TESE procedure has an open surgery that allows better target tissue expansion and checking of testicular tissues. This aids in a more selective and minutely controlled harvest which increases the chances of finding viable sperm in cases where sperm production is extremely meager.
In addition, Micro TESE is believed to be both a more specific and efficient way for men with severe infertility issues. This method is commonly recommended for patients with conditions such as non-obstructive azoospermia. It also promises a higher sperm retrieval success rate.

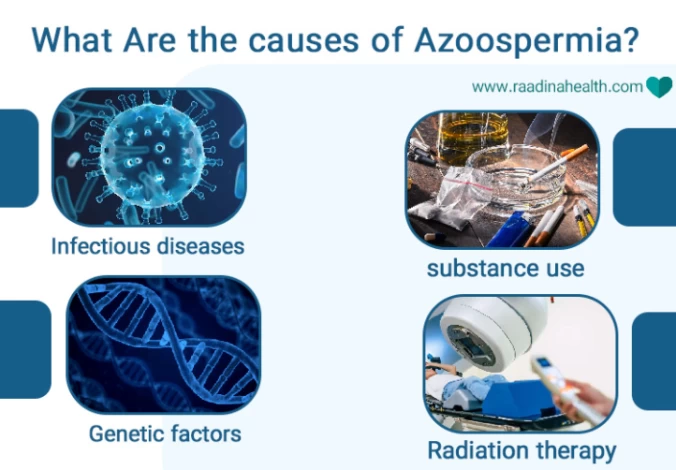
What Are the causes of Azoospermia?
Azoospermia, or zero sperm count, occurs for several reasons and is aggravated by various factors. Some factors affecting azoospermia include:
- Infectious diseases such as mumps;
- Taking some medications, especially drugs for chemotherapy and antibiotics;
- Radiation therapy in cancer patients;
- Genetic factors;
- Hormonal factors;
- substance use;
- Occurrence of genital ulcers.
What is the Micro-Tese Success Rate?
The success rate of Micro TESE varies depending on the patient's specific condition and the expertise of the surgeon performing the procedure. However, studies have shown that Micro TESE has a higher chance of successful sperm retrieval compared to traditional TESE. Micro TESE Success rates of 50-60% or even higher have been reported in some studies for infertile men undergoing this procedure.
For which type of patients with azoospermia is micro-TESE more successful?
Studies have shown a micro-TESE success rate of 50% for men with Klinefelter Syndrome. Klinefelter Syndrome is a male genetic condition that leads to smaller-than-normal testicle size, low testosterone levels, and the absence of sperm in the semen (azoospermia).
Micro-TESE also has a high success rate of sperm retrieval in patients who had orchiopexy surgery or in men with germ cell aplasia.
When is Microscopic Testicular Sperm Extraction Recommended?
Microscopic testicular sperm extraction (micro-TESE) is typically recommended in cases where a man has been diagnosed with severe male infertility, particularly if there is no sperm present in the ejaculate. This procedure is often used for men with conditions such as non-obstructive azoospermia, where the testicles are not producing enough sperm.
Micro-TESE procedure is also recommended when other methods of sperm retrieval, such as testicular sperm aspiration (TESA) or percutaneous epididymal sperm aspiration (PESA), have been unsuccessful.
Options for Fertility After Vasectomy
While vasectomy is an effective method of contraception, it is not always irreversible. In fact, up to 6% of men who undergo vasectomy may experience a reversal of the procedure due to changes in their personal circumstances, such as remarriage or a desire to have more children.
For men who have undergone vasectomy and wish to conceive a child, there are several options available. One option is vasectomy reversal surgery, which reconnects the vas deferens to allow the passage of sperm. However, this procedure is not always successful, and success rates have decreased over time since the original vasectomy.
Another option is sperm extraction with micro-TESE, which involves the removal of testicular tissue to retrieve viable sperm for use in assisted reproductive technologies. This method is successful in men who have undergone vasectomy, even if they have no sperm in their ejaculate.
Why Infertility Treatment in Iran?
Infertility treatment in Iran is also significantly more affordable compared to many other countries. The cost of procedures such as in vitro fertilization (IVF) and other fertility treatments in Iran can be much lower than in Western countries, making it an attractive option for individuals and couples seeking infertility treatment.
Additionally, Iran has highly skilled and experienced doctors in the field of infertility treatment, with many clinics and hospitals offering state-of-the-art facilities and advanced technology for assisted reproductive techniques. This combination of affordability and quality medical care has made Iran a popular destination for medical tourism for individuals and couples seeking infertility treatment.
FAQs About Micro-TESE Surgery
What are the Micro Side Effects?
In general, the chance of damaging the testicle itself during the surgery is very low because the scrotum heals quickly after surgery; however, micro TESE surgery side effects like bleeding, infection, pain and discomfort at the surgical site, swelling or bruising in the scrotum, and numbness or tingling in the scrotum may occur for the patient and should be reported to the doctor.
Is it OK to undergo a second micro-TESE if no sperm could be harvested in the first procedure?
In case of no sperm found in the first micro-TESE, the chance of harvesting sperm in a second procedure remains similarly low, around 15 to 20%.
Will the microscopic testicular sperm extraction procedure need to be repeated?
The need for repeated micro TESE procedures can vary from person to person depending on factors such as the underlying cause of male infertility, the quality of the sperm retrieved, and the specific requirements of the fertility treatment.
What is the success rate of micro-TESE surgery?
About 60% of doctors find Micro-TESE ideal, making it a good method for treating male infertility.
What type of anesthesia is used for the micro-TESE procedure?
Micro TESE surgery is typically performed under general anesthesia, which means the patient is completely unconscious during the procedure. This allows the surgeon to carefully and precisely locate and extract sperm from the testicular tissue without causing discomfort or pain to the patient.
 WhatsApp
WhatsApp
 Telegram
Telegram
 Facebook
Facebook
 Email
Email












No reviews
Your comment