Dysmenorrhea (Painful Menstrual Periods): Causes and Treatment
Fertility Treatment
Dysmenorrhea is a medical term used to describe painful menstrual cramps that occur before or during menstruation. The pain is typically felt in the lower abdomen, and can range from mild to severe. Statistics show that menstrual pain tends to lessen with age and after giving birth.
Dysmenorrhea is a common condition that affects many women and can be caused by various factors such as hormonal imbalances, uterine fibroids, or conditions like endometriosis. It typically lasts about 48 to 72 hours, until hormone levels in the body drop to zero around day 3 or 4 of the period. Treatment for dysmenorrhea may include pain relievers, certain home remedies, and other interventions to help manage the pain.
What Are the Types of Dysmenorrhea?
Menstruation occurs when the levels of progesterone and estrogen hormones decrease, leading to the shedding of the uterine lining. The excess tissue is expelled from the body through bleeding. If menstrual pain persists despite taking painkillers, it may indicate a condition known as dysmenorrhea.
There are two main types of dysmenorrhea: primary and secondary, each with distinct characteristics that we will elaborate on below:
There are two types of period cramps: primary and secondary.
Primary Dysmenorrhea
Primary dysmenorrhea typically starts with the first ovulatory cycles in young women and may continue throughout their life, possibly even into their fifties. It is usually due to an increase in prostaglandin levels, which causes the uterine muscles to contract more strongly, particularly in ovulatory cycles, and can lead to severe frequent menstrual contractions, low uterine blood flow, and sensitive pelvic nerves.
Secondary Dysmenorrhea
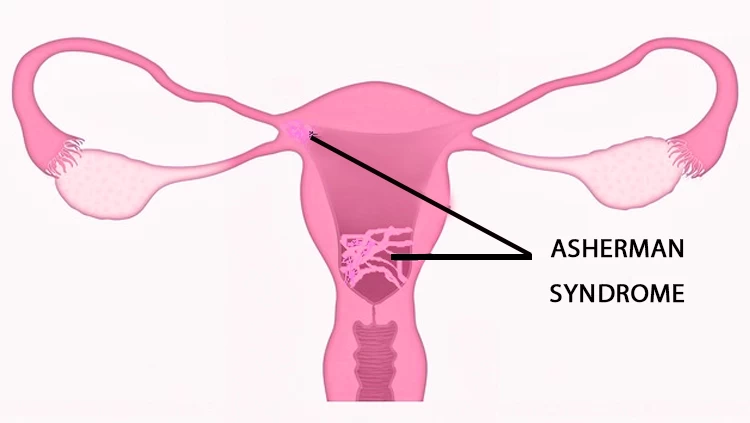
This type of dysmenorrhea is caused by an underlying medical condition, such as endometriosis, fibroids, pelvic inflammatory disease, or adenomyosis. These conditions can lead to inflammation, scarring, or abnormal tissue growth in the reproductive organs, resulting in painful menstrual cramps. It typically arises in anovulatory cycles and affects women aged between 35 and 45. Treatment for secondary dysmenorrhea focuses on addressing the underlying cause of the condition.
Who Might More Likely Have Dysmenorrhea?
You may have a higher risk of painful periods if:
- You started menstruating before the age of 12;
- You are under the age of 20;
- Your periods are exceptionally heavy or last longer than a week;
- You smoke;
- You have a parent who also suffers from dysmenorrhea.
What Are the Most Common Symptoms of Dysmenorrhea?
Dysmenorrhea, also known as menstrual cramping or colic, can cause discomfort in the middle and lower abdomen, lower back, inner thighs, and even the kidneys.
The common symptoms of painful periods may include:
- Diarrhea or loose stools;
- Nausea and vomiting;
- Fatigue;
- Headaches;
- Throbbing pain and severe cramping in the lower abdomen;
- Persistent pain during period;
- Pain that may radiate to the lower back and thighs;
- Pelvic pain;
- Dizziness or fainting.
What Are the Causes of Dysmenorrhea?
Some risk factors for dysmenorrhea may include:
- Irregular periods;
- Heavy menstrual bleeding;
- Young Age (under 30 years);
- A family history of painful menstruation;
- Not having children;
- Use of intrauterine devices (IUDs);
- Stress and anxiety;
- Lifestyle factors like poor diet, lack of exercise, smoking, and excessive alcohol consumption.
Conditions that can cause dysmenorrhea are as follows:
- Endometriosis: Endometriosis is a condition where the tissue that lines the inside of the uterus grows outside the uterus. This can lead to inflammation, scarring, and pain during menstruation.
- Adenomyosis: Adenomyosis is a condition where the tissue that lines the uterus grows into the muscular wall of the uterus, leading to inflammation and pain in the reproductive organs.
- Premenstrual syndrome: Premenstrual syndrome (PMS) refers to a combination of physical and emotional symptoms that occur a week or two before menstruation due to an increase in prostaglandin level. The pain caused by Premenstrual syndrome (PMS) decreases after the start of period bleeding.
- Fibroids: Uterine fibroids are noncancerous growths in the uterus that can cause abnormal pain and heavy menstrual bleeding.
- Ovarian cysts: Ovarian cysts are fluid-filled sacs that may form in or on the ovaries. When large, these cysts can lead to pain and discomfort, particularly during menstruation. Additionally, ovarian cysts have been linked to elevated levels of stress and anxiety. Fortunately, hormone therapy is an effective treatment option for managing ovarian cysts.
- Pelvic inflammatory disease (PID): PID is an infection of the female reproductive organs, often caused by sexually transmitted infections. It can lead to inflammation and pain during menstruation.
- Cervical stenosis: Cervical stenosis is a condition where the opening of the cervix is narrow, making it difficult for menstrual blood to pass through, leading to increased pressure and dysmenorrhea.
- Past Miscarriage: The physical trauma of experiencing a miscarriage can disrupt the normal hormonal balance and functioning of the reproductive system. This disruption may result in irregular menstrual cycles, increased intensity of menstrual cramps, and other menstrual-related symptoms, including dysmenorrhea.
What Are the Complications Associated with Dysmenorrhea?
Some potential complications of painful periods may include:
- Absenteeism from work or school: Severe pain during periods may cause individuals to miss out on work or school, leading to a decline in productivity and affecting their overall quality of life;
- Impaired daily activities: Painful periods can make it difficult for individuals to perform daily activities such as exercising, socializing, or completing household chores;
- Emotional distress: Chronic pain during periods can take a toll on an individual’s mental health, leading to feelings of anxiety, depression, and irritability;
- Relationship issues: Constant pain and discomfort during periods may impact an individual’s relationships with their partners, family members, or friends;
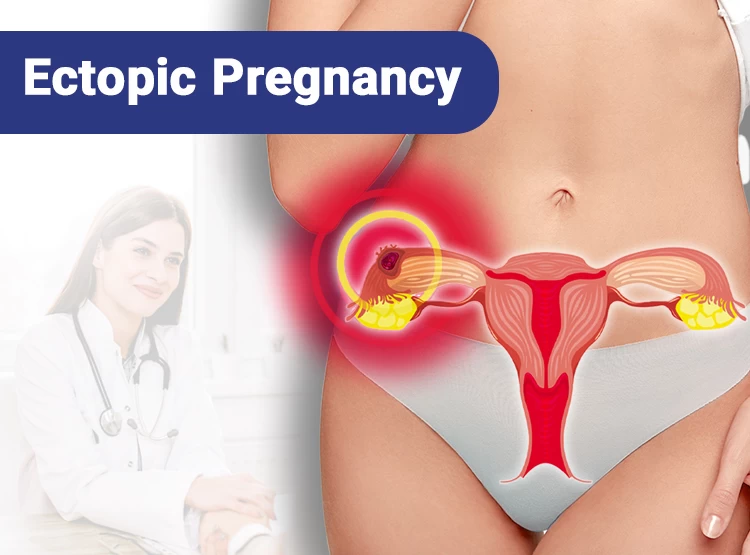
- Female infertility: In some cases, conditions such as endometriosis or pelvic inflammatory disease, which can cause painful periods, may also affect fertility.
How to Relieve Menstrual Pains?
Secondary dysmenorrhea can typically be managed with appropriate treatment. Some ways to help relieve painful periods can be:
Hormonal Birth Control Methods Such as Oral Contraceptives
Hormonal birth control pills can help regulate menstrual cycles and reduce menstrual pain for young women who want to prevent pregnancy. These pills can relieve severe menstrual contractions due to having specific doses of estrogen. They can also reduce the level of prostaglandin by preventing ovulation.
Hormonal birth control pills can effectively alleviate menstrual pain for young women seeking to prevent pregnancy. By containing specific doses of estrogen, these pills can reduce severe menstrual cramps. Additionally, they work to lower prostaglandin levels by preventing ovulation, providing further relief from menstrual discomfort.
NSAIDs and Other Pain Relievers
NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen and Mefenamic acid are commonly used to alleviate menstrual pain. While these medications can be effective, women need to avoid excessive consumption of aspirin and paracetamol due to potential risks.
What Are the Best Home Remedies for Dysmenorrhea (Painful Menstrual Cramps)?
Common treatments for Dysmenorrhea may include:
- Massaging the lower abdomen and back to alleviate muscle tension;
- Applying a heating pad or hot water bottle to the lower abdomen, waist and pelvis;
- Getting regular gentle exercises like walking, yoga, stretching exercises, or meditation;
- Consuming foods rich in magnesium, calcium, and omega-3 fatty acids, such as leafy greens, nuts, and fatty fish;
- Taking supplements containing vitamins E, B1 and B6;
- Drinking herbal teas like chamomile, ginger, or peppermint;
- Staying hydrated by drinking plenty of water to reduce bloating and cramps associated with menstruation;
- Taking antidepressants in some cases to reduce mood swings associated with premenstrual syndrome;
- Limiting the intake of caffeine, alcohol, and sugar to help prevent bloating;
- Following prescribed antibiotic treatment for conditions like pelvic inflammatory disease or sexually transmitted infections;
- Addressing underlying conditions such as ovarian cysts, endometriosis, or uterine fibroids that may be contributing to menstrual pain;
- Considering a hysterectomy (complete removal of the uterus) as a last resort if other treatment methods prove ineffective and future childbearing is not desired.
How to Treat Dysmenorrhea with Traditional Medicine?
Traditional medicine experts recommend consuming herbal teas made from chamomile, fennel, cinnamon, ginger, and dill to help alleviate severe menstrual pain. It is important to avoid combining herbal remedies with chemical medications. Additionally, acupuncture has shown to be effective in relieving menstrual pain.
Normal Cramps Vs. Dysmenorrhea
Normal cramps associated with menstruation are usually mild to moderate in intensity and occur before or during your period. They may feel like a dull ache or pressure in your lower abdomen and typically improve with over-the-counter pain relief medication, heat therapy, or rest. Dysmenorrhea, on the other hand, is a medical term for severe menstrual cramps that significantly interfere with daily activities and quality of life. These cramps are often accompanied by other symptoms such as nausea, vomiting, diarrhea, fatigue, and headaches. They usually start a few days before your period and can last for several days into your period.
When to See a Doctor for Menstrual Cramps?
It is important to see a doctor if you experience severe or debilitating menstrual pain that significantly impacts your daily activities or quality of life. Other reasons to seek medical attention for menstrual pain can include:
- Experiencing three or more consecutive painful menstrual periods;
- Heavy bleeding during your period;
- Persistent pelvic pain even after your menstrual period has ended, as it could indicate a possible infection that may lead to complications like infertility;
- Spotting or bleeding between menstrual cycles;
- Regularly experiencing symptoms like nausea, diarrhea, and abdominal cramps during each menstrual period.
Why Iran for Infertility Treatment?
Iran has emerged as a popular destination for infertility treatment due to its advanced medical facilities, skilled healthcare professionals, and affordable treatment options.
Iranian fertility specialists are renowned for their expertise in treating complex infertility cases and have helped numerous couples achieve their dream of starting a family. Additionally, the clinics in Iran adhere to strict quality standards and use the latest medical technologies to ensure the best possible outcomes for their patients.
Another factor that makes Iran an attractive option for infertility treatment is the relatively low cost of treatment compared to Western countries. The cost of fertility treatments in Iran is significantly lower, making it a more affordable option for couples who may be facing financial constraints. Despite the lower costs, patients can expect to receive high-quality care and personalized treatment plans tailored to their specific needs.
Furthermore, Iran is considered a safe and welcoming destination for international patients seeking infertility treatment. The country has a well-established medical tourism industry and is known for its warm hospitality and cultural richness. Many fertility clinics in Iran offer services specifically tailored to international patients, including assistance with travel arrangements, accommodation, and translation services.
Final Word
Menstrual pain is a common issue many women face. However, it may be a sign of dysmenorrhea when it becomes unbearable. While home remedies and the suggestions in this article can provide relief, seeking medical attention is crucial if the pain persists.
Consulting a doctor is essential to receive the most appropriate treatment, as severe period pains may indicate underlying conditions such as Pelvic Inflammatory Disease (PID) or sexually transmitted infections. Timely diagnosis and treatment of dysmenorrhea are vital for improving women's overall health and well-being.
FAQs on Dysmenorrhea
Is having dysmenorrhea normal?
Yes, having dysmenorrhea, or painful periods, is considered normal for many women. It is estimated that about 50% of women experience some degree of menstrual pain and discomfort. However, a healthcare provider should evaluate severe or debilitating pain to rule out any underlying conditions.
How is dysmenorrhea diagnosed?
Dysmenorrhea is typically diagnosed based on a woman's symptoms and medical history. In some cases, further tests such as ultrasound or laparoscopy may be needed to rule out other underlying conditions.
What is the main cause of painful periods?
The main cause of painful periods is the release of prostaglandins, which are hormone-like substances that cause the uterus to contract and shed its lining. This can result in cramping and pain during menstruation.
Can I prevent dysmenorrhea?
There is no sure way to prevent dysmenorrhea, as it is a common menstrual symptom experienced by many women. However, there are some steps you can take to potentially reduce the severity and frequency of menstrual cramps like maintaining a healthy lifestyle, following a balanced diet and getting regular exercise.
Is dysmenorrhea more common in certain age groups?
Dysmenorrhea is most common in adolescents and young women, with the highest prevalence occurring in women between the ages of 16 and 25.
Can dysmenorrhea cause infertility?
While dysmenorrhea itself does not cause female infertility, the underlying conditions that can cause dysmenorrhea may affect fertility.
For example, conditions such as endometriosis, pelvic inflammatory disease, and fibroids are all known to cause severe menstrual pain and can also impact fertility. If left untreated, these conditions can lead to scarring or damage to the reproductive organs, which can make it difficult to conceive.











No reviews
Your comment