Hysteroscopy Before IVF: Purpose & Procedure
Fertility Treatment
Hysteroscopy surgery is a simple and minimally invasive procedure that can diagnose or/and treat female uterine disorders. This diagnostic treatment method is usually performed under general anesthesia. The doctor inserts a hysteroscope (a thin tube with a small camera) into the vagina to examine the possible disorders of the cervix, vagina, and uterus (such as abnormal vaginal bleeding and painful periods).
Diagnostic hysteroscopy usually takes up to 30 minutes and does not require hospitalization. Read on to learn about different types of hysteroscopy, how and why they are performed, and the best candidates for them.
What Is a Hysteroscopy?
Hysteroscopy is a diagnostic-operative procedure to examine female genital problems. The doctor inserts a thin camera tube into the uterus through the vagina during this procedure. In some cases, the uterus may be filled with gas or liquid (carbon dioxide and low-viscosity fluids) to provide a clear field of view for the doctor. The doctor then examines the obtained images to find the cause of infertility and recurrent miscarriage. It should also be mentioned that this procedure is one of the steps of IVF, in which the doctor checks whether the uterus is healthy enough to hold the embryo.
Diagnosing and treating uterine polyps, fibroids, septum, scar tissue, and other abnormalities will be possible through hysteroscopy surgery. This minimally invasive procedure is also performed in assisted conception methods (such as IVF) along with other examinations and tests such as sperm analysis, FSH and LH tests, and STD tests.

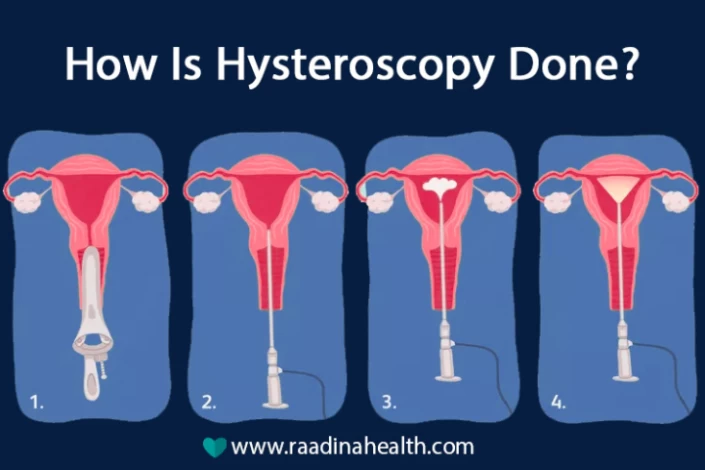
How Is Hysteroscopy Done and How Long Does Hysteroscopy Surgery Take?
Hysteroscopy does not usually require general anesthesia because no incision is made on the skin except in exceptional cases when the surgery is prolonged and more invasive.
Hysteroscopy may take 5 to 30 minutes. During this time, the patient wears unique clothes and lies on the examination bed. The doctor applies a sedative or general anesthesia to the diagnosis, and the procedure begins.
According to the NIH, "Next, the hysteroscope is set up, the camera is white-balanced and focused, and the inflow tract is primed. With the vaginoscopic entry technique, traditional instruments are not needed."
The doctor inserts a small speculum into the vagina, like a pap smear test, to keep the cervix open. Then, a narrow tube called a hysteroscope is inserted. A saline liquid or carbon dioxide gas is slowly released into the uterus to expand it and provide a better view of the inside for the doctor.
The hysteroscope contains a light and a tiny camera at its end, which can send images of the uterus, fallopian tubes, and cervix to the monitor. It can also be used to collect cell samples for biopsy. If surgery is needed, the surgical instruments are inserted into the uterus through the hysteroscope. Therefore, the doctor can observe the uterine cavity and its surroundings and diagnose and treat adhesions and all uterine masses.
According to NIH, "AUB (Abnormal Uterine Bleeding) is the most common indication for hysteroscopy with structural abnormalities such as polyps and/or fibroids, usually as root causes."
How to Prepare for Hysteroscopy?
Some necessary measures and care that should be done before performing hysteroscopy surgery are as follows:
- Perform all required tests, including pregnancy tests and blood tests;
- Take medicine according to the doctor's advice to check detected fibroids;
- Use contraceptives to prevent pregnancy until the completion of hysteroscopy treatment;
- Take medicines such as ibuprofen around an hour before the surgery to reduce post-surgery pain;
- Prepare for local anesthesia on the cervix;
- Prepare for general anesthesia in cases such as treatment of fibroids with hysteroscopy;
- If general anesthesia is required, stop eating and drinking for a few hours before surgery.
After Hysteroscopy: What to Expect?
Some aftercare measures should be taken to help speed up the recovery process after hysteroscopy, including:
- Rest for several hours or a day and then return to routine activities;
- Rest for several days in case of having general anesthesia;
- Do not drive after hysteroscopy with general anesthesia;
- Have a healthy diet;
- Be prepared for uterine contractions and abdominal pain (such as menstrual pain), the feeling of gas accumulation in the lower abdomen for up to 24 hours, vaginal spotting and bleeding for several days;
- See a doctor in case of severe pain or abnormal bleeding;
- Avoid sexual intercourse until the bleeding and spotting stop (at least 1 to 2 weeks after the surgery) to reduce the risk of infection;
- Take medications prescribed by the doctor.

What Are the Different Types of Hysteroscopy?
One of the most common reasons for performing hysteroscopy is to diagnose the cause of abnormal uterine bleeding due to irregular periods.
There are generally two types of hysteroscopy: diagnostic and operative.
Diagnostic Hysteroscopy
Diagnostic hysteroscopy is used to identify uterine problems, diagnose the causes of female infertility, and confirm the results of tests such as hysterosalpingography (HSG, a colour X-ray test to evaluate the uterus). This type of hysteroscopy is sometimes performed with laparoscopy or before dilation and curettage (D&C procedure), also known as hysteroscopy D&C.
Some of the common uses of diagnostic hysteroscopy are as follows:
- Finding the cause for repeated miscarriages;
- Examining female infertility and its causes;
- Diagnosing polyps and fibroids (non-cancerous tumors of the uterus);
- Examining the condition of the uterus during the IVF process and before embryo transfer;
- Investigating the cause of pelvic pain.
Operative or Therapeutic Hysteroscopy
Operative hysteroscopy treats the abnormalities or disorders identified in diagnostic hysteroscopy, which is sometimes performed together. During therapeutic hysteroscopy, surgical tools are inserted into the uterus through the hysteroscope to improve uterine disorders.
The most common uses of operative hysteroscopy are as follows:
- Locating an IUD for preventing pregnancy;
- Removing uterine adhesions caused by surgery and infection that will result in absent period and female infertility;
- Performing a biopsy to take a sample of tissue;
- Removing polyps or fibroids.

Why Is Hysteroscopy Done?
Both types of hysteroscopy (operative and diagnostic) are used for various reasons. Some of their uses are to diagnose disorders and confirm other tests. The procedure is also sometimes used to treat gynecological disorders.
The most common reasons for performing hysteroscopy are as follows:
- Diagnosis and treatment of tumors;
- Diagnosis and treatment of endometrial diseases;
- Diagnosis and treatment of uterine malformations;
- Diagnosis and treatment of vaginal bleeding causes;
- Helping the IVF process;
- Dilation and evacuation or D&E.
Other Uses of Hysteroscopy
In general, the common uses of hysteroscopy surgery are as follows:
- Investigating menorrhagia (heavy menstrual bleeding);
- Investigating prolonged menstrual bleeding;
- Measuring postmenopausal bleeding;
- Investigating abnormal bleeding between periods;
- Diagnosing and treating polyps, myomas, fibroids, and intrauterine adhesions;
- Diagnosing the cause of abnormal results from pap smear test;
- Diagnosing symptoms of repeated (more than one) miscarriages;
- Removing the IUD device (a device used for preventing pregnancy);
- Collecting cell samples for biopsy;
- Completing the laparoscopy;
- Diagnosing uterine malformations;
- Re-checking the uterus and scratching the endometrium before embryo transfer;
- Removing the remains of the dead fetus before D & C.
Hysteroscopy before IVF embryo transfer
Hysteroscopy can diagnose the cause of repeated IVF or implantation failure. Performing this procedure before IVF may also help increase the treatment's success. During a Hysteroscopy, the endometrium is scratched before the embryo transfer, increasing the chance of implantation.
What Is Endometrial Scratching Technique Before IVF?
Endometrial scratching is a widely used technique to increase the chance of pregnancy in women undergoing IVF treatment, during which the inner layer of the uterus is scratched. Endometrial scratching can be performed with procedures such as hysteroscopy and endometrial biopsy.
The purpose of endometrial scratching is to cause slight damage to the uterus lining and encourage the body to repair the endometrium by releasing white blood cells and growth factors. This makes the endometrium a better place for embryo implantation. Therefore, the chemicals released during endometrial scratching help the embryo connect to the uterus.

What Is Endometrial Scratching with Hysteroscopy?
Endometrial scratching during hysteroscopy is a procedure done vaginally (without making an incision on the abdomen) and under general anesthesia. During this procedure, the doctor can diagnose and treat conditions such as fibroids or polyps and create a scratch on the uterus.
The aim of endometrial scratching during hysteroscopy is to increase the success of embryo implantation. During hysteroscopy, the best time to scratch the uterus is before the embryo transfer stage (day 5 to day 7 of IVF treatment).
How Does Endometrial Scratching Affect the Success of IVF Embryo Transfer?
Endometrial scratching can increase the chance of embryo transfer success in IVF by two times. On the other hand, as endometrial scratching is a minimally invasive procedure with a low risk of pain and infection, it is recommended for patients with high-quality embryos but failed IVF. The reason is that there may be a possibility of endometrium conditions in patients with high-quality embryos who experienced IVF failure.
It should be said that endometrial scratching may not lead to a positive and successful result in women of advanced age or patients with low-quality and sick embryos (in terms of genetic problems and chromosomal abnormalities). Therefore, it is better to perform pre-implantation genetic tests before endometrial scratching to ensure the health and quality of the embryo and the suitability of this method.
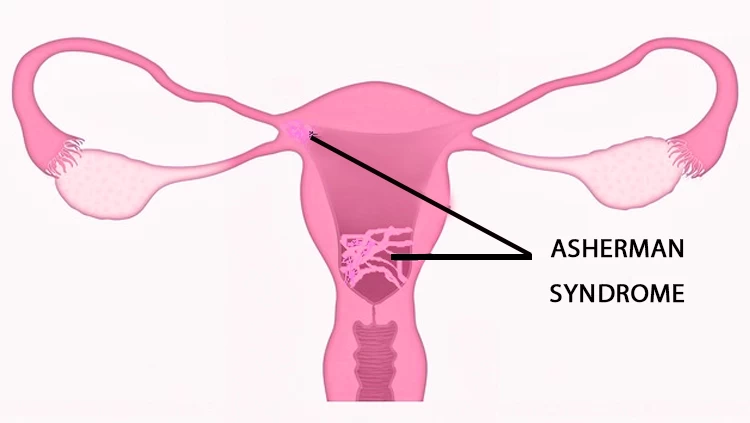
Diagnosing and Treating Asherman Syndrome with Hysteroscopy
Asherman syndrome, also known as intrauterine adhesions, is a condition characterized by the formation of scar tissue within the uterine cavity, often resulting from surgical procedures like dilation and curettage (D&C). This scar tissue can cause infertility, menstrual irregularities, and recurrent pregnancy loss. Hysteroscopy plays a crucial role in both diagnosing and treating Asherman syndrome. During this procedure, a thin, lighted instrument called a hysteroscope is inserted through the cervix into the uterus, providing direct visualization of the uterine cavity. This allows clinicians to identify the location and extent of the adhesions accurately.
Furthermore, hysteroscopy enables the precise removal of these adhesions using specialized instruments, often in the same session. Post-operative care may include hormonal treatments to aid in the regeneration of the endometrial lining and prevent the recurrence of adhesions. Through the minimally invasive approach of hysteroscopy, women with Asherman syndrome can experience significant improvements in their reproductive health and chances of conceiving.
What Are the Complications of Hysteroscopy?
Hysteroscopy is a minimally invasive diagnostic and operative method that may become more invasive when combined with other treatment methods.
The complications of hysteroscopy can be as follows:
- Problems caused by anesthesia and general anesthesia;
- Uterine infection;
- Accumulation of fluid and gas in the uterus;
- Embolus caused by electrolyte imbalance;
- Damage to the cervix and the uterus;
- Pelvic inflammatory disease (PID) has symptoms such as severe abdominal pain, fever, and severe vaginal bleeding;
- Uterine perforation (Rare);
- Peritonitis (inflammation in the peritoneum).

When Is the Best Time to Perform Hysteroscopy?
The best time to perform a hysteroscopy is one week after the end of the period cycle when the condition of the uterus and other organs is more evident to the doctor.
It is recommended that patients take birth control pills from day 5 of their period to 2-3 days after the end of menstrual bleeding before performing hysteroscopy. It should be noted that hysteroscopy does not have a time limit for postmenopausal women. If you are getting hysteroscopy to remove fibrosis before starting the IVF process, you should wait two to 12 weeks before starting the cycle.
How Much Does Hysteroscopy Cost?
The cost of diagnostic and operative hysteroscopy procedures depends on the clinic or hospital's price, the surgeon's salary, and the cost of complementary and alternative therapies. However, hysteroscopy is slightly more expensive than open surgery. In Iran, the price of this operation ranges between 1,000 and 2,000 USD, which covers the surgeon’s fee, hospital charges, and pre-and post-op medications.
The Bottom Line
Hysteroscopy is an effective and low-risk procedure for diagnosing and treating uterine diseases or abnormalities of the female reproductive system. This procedure is used widely due to its minimal invasiveness and short-term recovery. Although hysteroscopy may cause risks in pregnant women or those suffering from uterine diseases, it is better to use it cautiously.
Frequently Asked Questions About Hysteroscopy
How long should I wait after hysteroscopy?
Most women can resume normal activities within 1–2 days, but heavy exercise or sexual activity should be avoided for about 1 week to allow the uterus to heal.
Why is hysteroscopy done before IVF?
Hysteroscopy is performed before IVF to check the uterine cavity for polyps, fibroids, scar tissue, or other abnormalities that could reduce implantation success.
How long should I wait to get pregnant after hysteroscopy?
In most cases, pregnancy can be attempted in the next menstrual cycle, but your doctor may advise waiting 2–4 weeks depending on the findings and any procedures performed during hysteroscopy.
Can hysteroscopy cure infertility?
Hysteroscopy can help diagnose and treat infertility causes such as polyps, myomas, and adhesions.
Is it possible to get pregnant after a hysteroscopy?
Yes! The chance of pregnancy after hysteroscopy is higher because this procedure can remove uterine tumours and abnormalities and check the health of fallopian tubes.
How much do I rest after a hysteroscopy?
Hysteroscopy does not require absolute rest. However, unnecessary activities should be avoided for 24 hours if the patient feels extremely tired. It is better to rest for a few days after undergoing hysteroscopy surgery (with general anesthesia).
How long should I wait to do embryo transfer after hysteroscopy?
There is no definite and exact interval between hysteroscopy and embryo transfer. The doctor advises this time, depending on the patient's condition. When performing a diagnostic hysteroscopy, the patient can get pregnant immediately in the next IVF cycle. However, it is better to wait at least one or two months before trying to get pregnant if hysteroscopy surgery is performed.
Will there be changes in my period after hysteroscopy?
It is common for women to experience changes in their menstrual cycles after a hysteroscopy. Some may notice lighter or heavier periods, irregular bleeding, or spotting. These changes are usually temporary and should resolve within a few cycles. However, if you have any concerns or the changes persist for an extended period, consult a healthcare provider.
How Painful Is a Hysteroscopy without Anesthesia?
Women do not experience the same degree of pain during hysteroscopy. This procedure is painless or causes little pain in most cases, but it can be easily controlled and tolerated by taking pain relievers prescribed by the doctor. Patients can also use pain relief drugs with the doctor's advice before hysteroscopy. However, the doctor can stop the procedure if patients feel severe pain.
How long to wait for frozen embryo transfer after hysteroscopy?
The recommended period after a hysteroscopy before undergoing a frozen embryo transfer (FET) varies depending on the reason for the hysteroscopy and the severity of any findings. Generally, a few weeks of recovery (up to three months) is advised, allowing the uterine lining to heal and reducing the risk of complications.














No reviews
Your comment