What are the Symptoms of Endometriosis?
Fertility Treatment
Endometriosis is a complex disease of the female reproductive system in which tissue similar to the lining of the uterus grows outside the womb. This disease can cause pain, fertility problems, severe menstrual cramps, menstrual delay, severe pain during and after sexual intercourse, and bowel problems. In this article, we discuss different symptoms and treatments of this disease and answer some of your frequently asked questions.
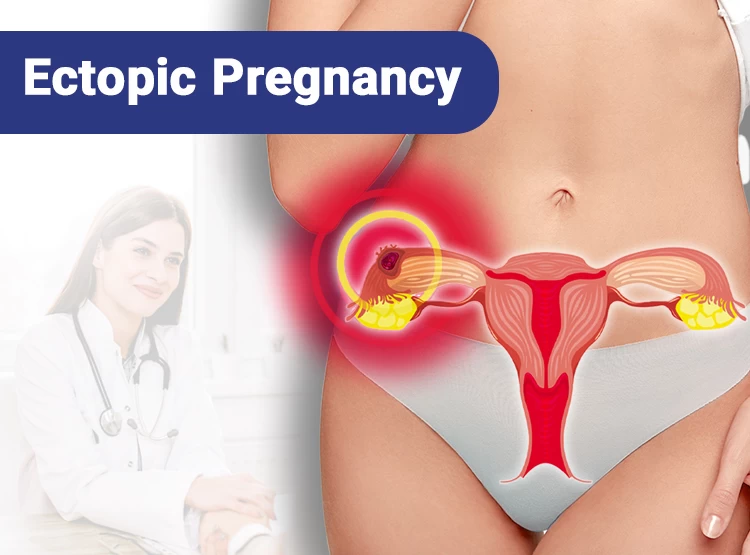
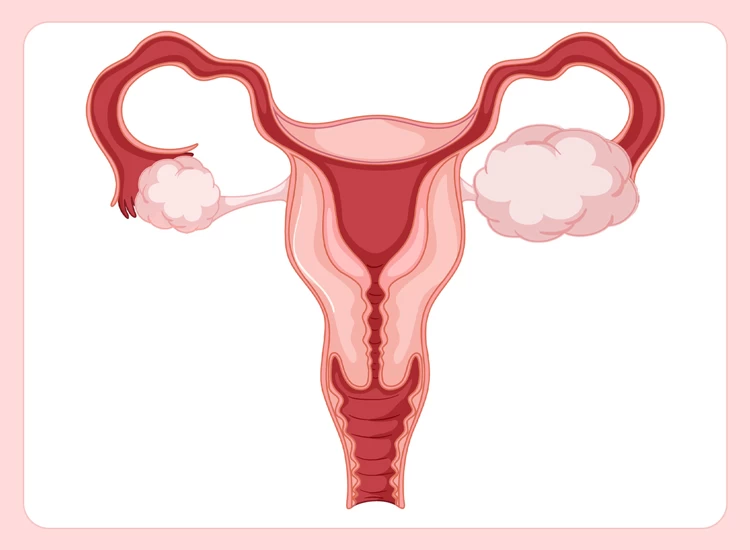
What Is Endometriosis?
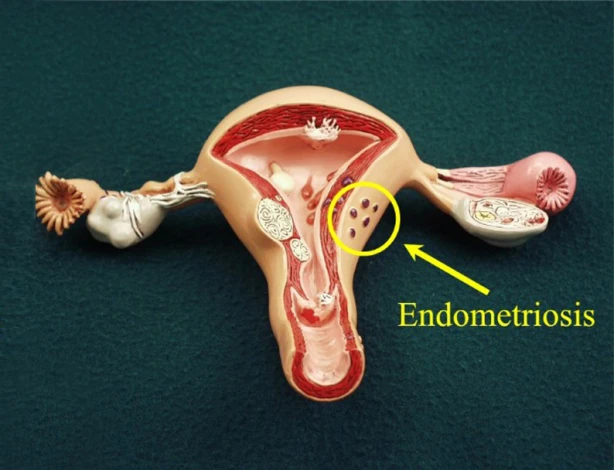
One of the most common diseases in women is endometriosis, the abnormal growth of uterine tissue outside the uterus. Mainly, this tissue is formed in the pelvis, ovaries, fallopian tubes, peritoneum, and the wall separating the anus and pelvis. We should note that endometriosis can also grow on cesarean wounds, laparoscopy wounds, bladder, intestine, appendix, and anus. The most crucial symptom of endometriosis is severe pain in the pelvic area. This pain often occurs during the menstrual cycle and sometimes before or after.
It should be noted that the upper transient tissue of the uterus sheds during menstruation, but this does not happen if the tissue is formed outside the uterus. As a result, endometriosis can have a wide range of side effects on the body. Complications of endometriosis include the obstruction of the fallopian tubes, difficulty in having sexual intercourse, difficulty in daily activities and working, and infertility.
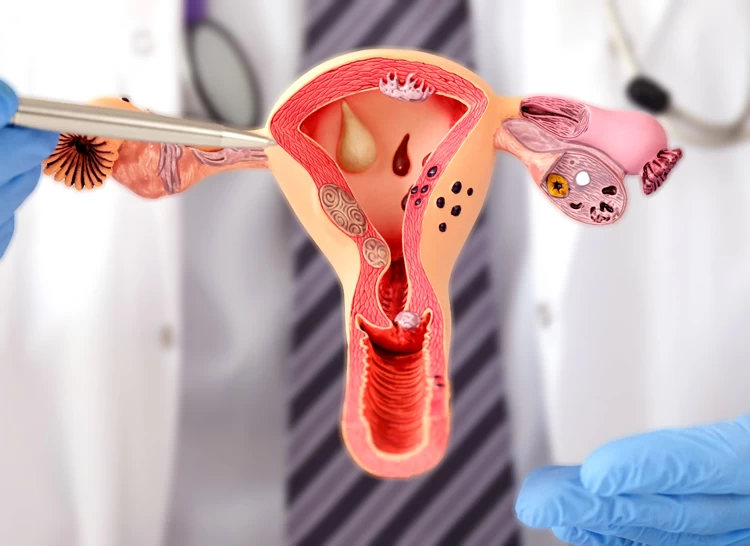
Endometriosis Stages
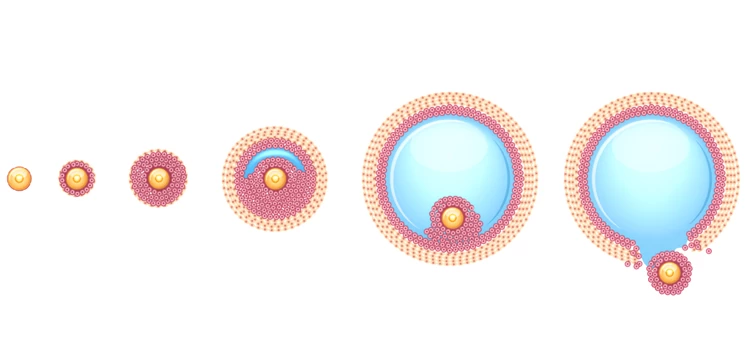
Endometriosis occurs in four stages; therefore, it has four symptoms and complications. The stages of endometriosis are determined according to the tissue's location, size, number, and depth. In the following, the four stages of endometriosis are introduced.
Stage 1 Endometriosis (Minimal)
At this stage of endometriosis, the endometrial tissue is shallow, and the severity of the disease is very low. In minimal endometriosis, these problems may occur:
- Inflammation in and around the pelvic cavity;
- The emergence of minor wounds inside the ovaries;
- Irritation in the intestines and bladder;
- Pain during sex;
- Painful periods and
- Excessive menstrual bleeding.
Stage 2 Endometriosis (Mild)
The symptoms of mild endometriosis are the same as minimal endometriosis but with deeper endometrial layers. Since light lesions are formed in the ovaries and pelvis during mild endometriosis, the last two weeks of the menstrual cycle are more painful. Also, you may experience pain during or after sex and while urinating, nausea, constipation, or diarrhea when you have stage 2 endometriosis.
Stage 3 Endometriosis (Moderate)
In moderate endometriosis, more lesions are formed, and the depth of endometrial tissue in the ovaries and pelvic lining also increases. At this stage, some cysts and adhesions are formed in one or both ovaries that cause severe pain in the pelvis and abdomen.

Stage 4 Endometriosis (Severe)
In stage 4 endometriosis, the lesions are implanted in the pelvis, ovaries, intestines, and fallopian tubes. The more endometriosis layers increase, the more pain and digestive problems increase; therefore, removing cysts is necessary.
It should be noted that severe cases of endometriosis can lead to infertility as it causes problems such as low egg quality, inflammation of the fallopian tubes, and adenomyosis or heterogeneous myometrial. However, mild to moderate endometriosis does not usually cause infertility.
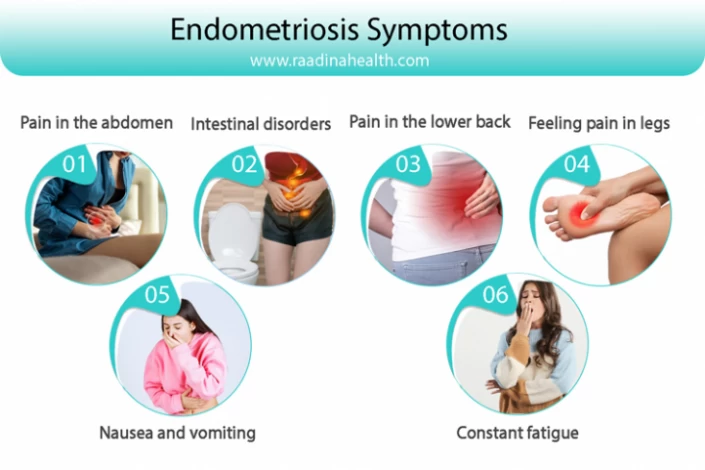
Endometriosis Symptoms
The first and most common sign of endometriosis is pain in the pelvis, especially during menstruation. This pain may occur in different areas and at different times. Some other symptoms of endometriosis include:
- Pain in the abdomen during menstruation that cannot be controlled by common painkillers such as ibuprofen;
- A menstrual period that lasts more than seven days;
- Severe bleeding accompanied by blood clot discharges during the menstrual period;
- Menstrual cycle less than 27 days;
- Pain in the lower abdomen during urinating or bowel movement;
- Intestinal disorders and irritable bowel syndrome (IBS) with symptoms such as diarrhea, constipation, stomachache, and bloating;
- Pain during or after sex;
- Chronic pain in the lower back;
- Nausea and vomiting;
- Constant fatigue;
- Pain during examination by a doctor;
- Depression;
- Bleeding and spotting between menstrual periods;
- Painful intestine movements and bleeding when defecting; and
- Feeling pain in legs.
In some cases, the above signs of endometriosis are caused by other diseases such as ovarian cysts, pelvic inflammatory disease (PID), or irritable bowel syndrome (IBS). Therefore, the main causes of such symptoms should be carefully determined before doing any treatment.
What Does Endometriosis Feel Like?
Many patients have declared that the pain of endometriosis is similar to that of the menstrual period but sharper and more severe. In endometriosis, the cramps are like stabbing in the stomach, and the patient cannot control them by taking regular OTC painkillers. Also, women with endometriosis have intolerable pain in the pelvis and belly during and -even two days- after sexual intercourse.
When Does Endometriosis Pain Occur?
In almost all cases, the endometriosis pain emerges two or three days before menstruation and continues for a few days afterward. Also, in some women, the pain occurs during and after sex, during bowel movement and urinating, while exercising, and between two periods.
Where Is Endometriosis Pain Located?
In most cases, endometriosis pain is not located in a certain location, and the patient feels it in different body parts. In general, endometriosis’s pain is located in one of the following parts:
- Bowel;
- Fallopian tubes;
- Ovaries;
- Uterus and other areas surrounding the uterus;
- The lower back;
- Pelvic area;
- Intestine;
- Bladder;
- Thighs;
- Neck and shoulders.
What Causes Endometriosis?
The leading causes of endometriosis are still unknown. However, scientists believe that estrogen will worsen endometriosis. That's why estrogen-regulating drugs are used to treat endometriosis. In addition to estrogen production, other factors cause endometriosis, such as:
- Genetic or inherited problems;
- Growth of stem cells in the pelvic and gastric mucosa;
- Transfer of endometrial cells by the lymphatic system to different parts of the body;
- Immune system disorders;
- Deformation of embryonic stem cells into endometrial-like cells due to stimulation of some hormones such as estrogen;
- The problem in menstrual blood flow that causes its entry into the pelvis or fallopian tubes instead of leaving the body;
- Being over the age of 35 years;
- Not exercising;
- Drinking too many caffeinated and alcoholic beverages;
- Low body mass index (BMI);
- Early menstruation;
- Late menopause;
- Genital disorders, etc.

Complications of Endometriosis
Endometriosis, as one of the most common and complicated diseases in women, has multiple complications such as:
- Diarrhea and constipation;
- Bloating and nausea;
- Severe or irregular bleeding during menstruation;
- Infertility;
- Cramping;
- Ovarian cysts;
- Intestinal and bladder problems such as ileus;
- Increased risk of ovarian and breast cancer;
- Rupture of cysts and lesions;
- Adhesion and scarring of internal tissues; and
- Inflammation of the surrounding areas of endometriosis.
Who Is More Likely to Get Endometriosis?
People with a family history of endometriosis are more likely to get this disease. Also, women who:
- Are between the ages of 25 and 35,
- Have no account of childbearing,
- Had endometriosis in the past,
- Have irregular periods longer than seven days with interval of fewer than 27 days and
- Undergone menstruation before the age of 12.
Endometriosis is highly dependent on sex hormones such as estrogen; therefore, reproductive age increases women's risk of developing this disease.
How Is Endometriosis Diagnosed?
There are several ways to diagnose endometriosis and its severity. Some lead to a definitive diagnosis of the disease, and some rule out the possibility of other conditions.
Some ways of diagnosing endometriosis include:
- Endometriosis ultrasound
- Having a detailed medical history
- Pelvic examination
- Differential diagnoses
- Laparoscopy and biopsy
- MRI
- Blood test
Endometriosis ultrasound
The doctor can perform a transvaginal or transabdominal ultrasound to diagnose the endometriosis in the uterus, ovaries, bladder, and intestines.

Having a detailed medical history
Doctors recommend patients report their problems, such as painful menstruation, pain during intercourse, and spotting before menstruation, to the doctor.
Pelvic examination
Clinical examinations of the pelvis and the surrounding organs are essential in identifying the early signs of Endometriosis.
Differential diagnoses
Doctors can diagnose Endometriosis by comparing its symptoms with other diseases with similar signs, such as ovarian cysts, pelvic inflammatory disease (PID), and irritable bowel syndrome with common symptoms such as abdominal pain, diarrhea, constipation, etc.
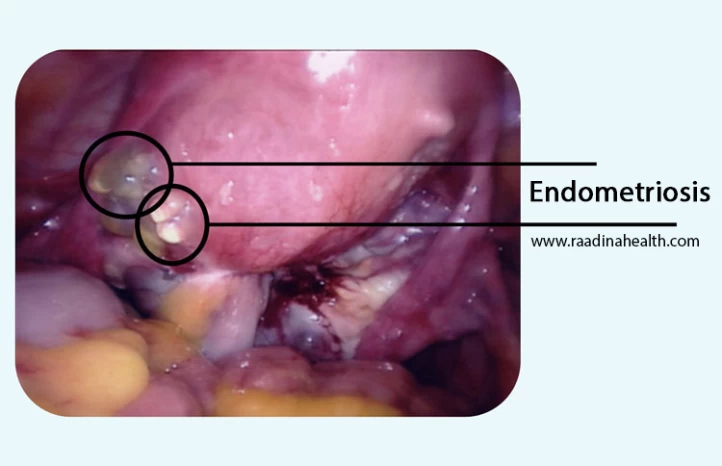
Laparoscopy and biopsy
Laparoscopic surgery and biopsy of the internal organs is the only definitive way to diagnose Endometriosis. Laparoscopy can determine the size, location, and depth of endometriosis.

MRI
By imaging the internal organs of the pelvic cavity and observing their condition, the doctor can detect the development of endometriosis.
Blood test
A blood test is ineffective for diagnosing endometriosis, but doctors may use it to check hormones.
Endometriosis Treatment
Since the causes of endometriosis are not yet known, there is no definitive treatment for it. However, most physicians suggest one of the following treatments to the patients based on their disease's severity, symptoms, age, and desire to have children in the future.
In the following, we introduce the most common methods of treating endometriosis and endometriosis medication:
- Dietary modification
- Taking analgesics
- Laparoscopy
- Laparotomy
- Hormone therapy
- Removing the ovaries and uterus
- Progestin therapy
- Taking gonadotropin-releasing hormone (Gn-RH) agonists
- Using ARTs
Dietary modification
People with endometriosis should avoid fatty foods, red meat, and animal by-products because these foods can increase estrogen production.

Taking analgesics
The doctors usually ask the patients to take nonsteroidal anti-inflammatory drugs such as naproxen, ibuprofen, and mefenamic acid to reduce their pain during menstruation.
Laparoscopy
As the most common treatment for endometriosis, laparoscopy aims to remove mild to severe tissues with the least complications possible. In this surgery, the surgeon makes micro incisions in the abdomen (usually in the belly button) and inflates it with gas to have a better view of the belly. Then, they insert a narrow tube with a tiny camera into the body to locate the endometrial tissue. After finding the exact area of endometriosis, the surgeon cuts it with microscopic surgical tools and removes the laparoscope and the instruments from the body.
Although this surgery improves the endometriosis symptoms to a great extent, it is done under general anesthesia and has a two-week downtime. So, you must take at least 10 days off from work and follow post-operative instructions to minimize anesthesia complications.
Laparotomy
Being more invasive than laparoscopy, this method is less common in treating endometriosis. In this operation, the surgeon makes a larger cut across the abdomen to remove severe and large endometrial tissues. The recovery period of laparotomy takes four to six weeks and involves more pain and discomfort.
Hormone therapy
By taking hormonal medications, the amount of estrogen in the body gets balanced, and therefore, the pain of endometriosis is reduced to a great extent.

Removing the ovaries and uterus
Removing the ovaries (oophorectomy) and uterus (hysterectomy) is the last option in treating endometriosis because the patient cannot get pregnant after these surgeries.
Progestin therapy
Subdermal progestin implants, levonorgestrel intrauterine devices (IUD), injectable contraceptives, and progestin pills stop the growth of endometrial tissue.
Taking gonadotropin-releasing hormone (Gn-RH) agonists
Taking these medications lowers estrogen levels, stops the production of ovarian-stimulating hormones, and prevents menstruation; as a result, the endometrial tissue will shrink.
Using ARTs
Sometimes, assisted reproductive techniques such as IVF or IUI treat endometriosis-related infertility.

Endometriosis and Infertility
About 30 to 50% of women with endometriosis have fertility problems because this disease causes:
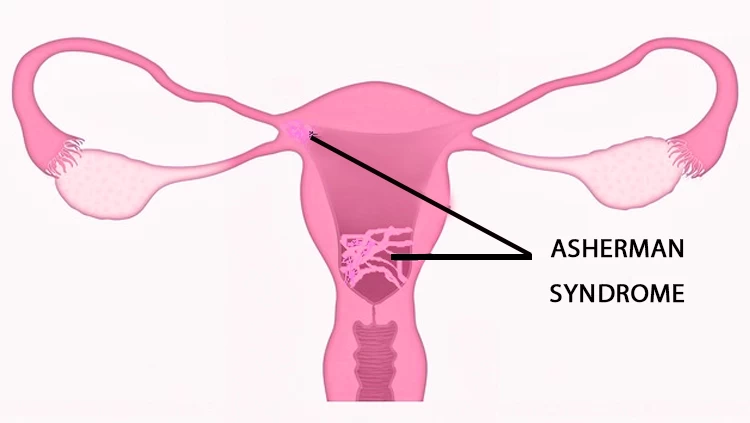
- Adhesion and scarring in the uterus;
- Limitation in egg growth;
- Reduction in egg production and quality;
- Disorders in the ovulation process;
- Changes in the pelvic anatomy;
- Pelvic inflammation;
- Hormonal imbalance; and
- Blockage of the fallopian tubes.
As it was mentioned above, most women with endometriosis have ovulation problems. For this reason, the doctor may prescribe fertility and ovulation induction drugs. As soon as ovulation begins, the doctor uses IVF or IUI procedures to increase the chance of pregnancy.
We should note that some treatments for endometriosis can prevent pregnancy or cause congenital disabilities; therefore, the whole treatment process should be done under the supervision of a skilled and experienced physician. Treatment for endometriosis to treat infertility is also time-consuming, so it should begin without delay.
Endometriosis and Recurrent Miscarriage
Endometriosis can lead to inflammation and scarring in the reproductive organs, affecting the implantation of the embryo and proper development of the pregnancy and cause recurrent miscarriage. Additionally, endometriosis can also impact the quality of the uterine lining, making it difficult for a fertilized egg to implant and grow properly.
Women with endometriosis who experience recurrent miscarriage may benefit from a multidisciplinary approach to care. This may include working closely with a reproductive endocrinologist, gynecologist, and possibly a fertility specialist to address any underlying issues that could be contributing to recurrent pregnancy loss.
Treatment options for women with endometriosis and recurrent miscarriage may include hormonal therapies to regulate the menstrual cycle, surgical interventions to remove endometrial lesions, and assisted reproductive technologies such as in vitro fertilization (IVF) to improve the chances of a successful pregnancy.
Endometriosis and Uterine Cancer
The relationship between endometriosis and uterine cancer has not yet been found. Endometriosis does not cause uterine cancer in all patients, but some cancers, such as breast cancer, are more common in women with this disease.
Uterine or endometrial cancer, which starts from the endometrial tissue, shows symptoms such as bleeding and spotting after menopause, between menstrual periods, and pelvic pain. Chronic inflammation and estrogen stimulation in patients with endometriosis increase the risk of endometrial cancer. So, if you notice any of the mentioned symptoms, visit your doctor and get a complete checkup before it's too late.
Contact us for a free initial consultation about fertility treatments
WhatsAppTelegramFacebookEmailFAQs about Endometriosis
1) Is endometriosis common?
Generally, %11 women between the ages of 15 and 40 have endometriosis. This disease appears and reaches its highest point in the third decade of women's lives.
2) Does endometriosis get better after menopause?
In most cases, the severe pain of endometriosis reduces after menopause because the body does not produce estrogen anymore. However, if the symptoms of endometriosis continue after menopause, they should be surgically treated.
3) Can you get pregnant with endometriosis?
Although endometriosis damages the egg cells and causes hormonal imbalance, it does not necessarily cause infertility. However, women with endometriosis have more complicated pregnancies and a higher rate of miscarriage.
4) Does endometriosis get better after having a baby?
It depends on each individual's body. Many women won't experience endometriosis symptoms as long as they are breastfeeding and not menstruating.
5) Can I prevent endometriosis?
Generally speaking, No. You cannot prevent endometriosis, but if you have a family history, you can lower its risk by controlling and reducing the estrogen level in your blood. To do so, you should reduce the intake of alcohol, caffeine, and red meat intake and exercise regularly.





















No reviews
Your comment