Testes Disorders: How Do they Affect Male Fertility?
Fertility Treatment
he function of the testes is to make sperm (male sex cells) and produce male hormones such as testosterone. Testicles are very sensitive to temperature and may seriously be damaged or lose their efficiency permanently if exposed to high temperature or even body temperature (37 degrees Celsius). Therefore, the testicles are located inside the scrotum outside the body.
Most testicular disorders are curable and rarely become severe. The probability of male infertility due to these testis problems is also low. However, men should visit a urologist if they see any changes in their testicles or feel pain or heaviness in their scrotum. Furthermore, they should avoid postponing this important matter due to embarrassment or anything else because testes disorder can lead to sexual dysfunction, hormonal imbalance, and male infertility.
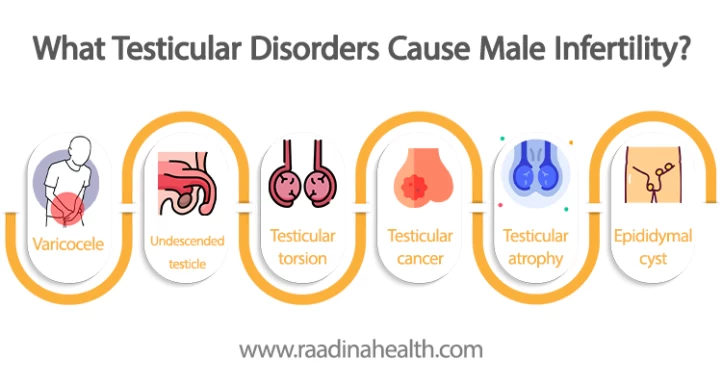
The most dangerous testicular disorders that can contribute to male infertility include severe cases of varicocele, undescended testicles (cryptorchidism), testicular torsion, testicular atrophy, and testicular cancer. These conditions can disrupt sperm production, quality, or the overall functioning of the reproductive system, ultimately impacting male fertility.

How Is the Anatomy of the Testes?
The testicles, also known as male sex glands, are two small oval-shaped sensitive organs behind the penis inside a sac-like skin called the scrotum. Each testis contains coiled tubes called seminiferous tubules.
There are also cells adjacent to the seminiferous tubules in the testes responsible for producing male hormones such as testosterone. Although, it should be noted that luteinizing hormone (LH) controls testosterone production. LH is also necessary for spermatogenesis (production of sperm) along with follicle-stimulating hormone (FSH).
After joining each other, the seminiferous tubules form a mesh-shaped network called the testicular network. This testicular network is connected to a crescent-shaped spiral tube called the epididymis, where the sperms are poured after production. The epididymis is where the sperm matures and is stored. It is located on the back and along the top of the testicles and acts as an interconnection between the vas deferens and the ejaculatory duct for transiting sperm.
Since producing high-quality sperm requires a temperature lower than body temperature, the testicular temperature should always be 2 to 3 degrees Celsius lower than the core body temperature.
What Testicular Disorders Cause Male Infertility?
Some testicular diseases can affect male infertility. Here is the testis disease list. We will explain each with their treatment options as follows.
- Varicocele
- Undescended testicle
- Testicular torsion
- Testicular cancer
- Testicular atrophy
- Epididymal cyst
- Hydrocele
- Hypogonadism
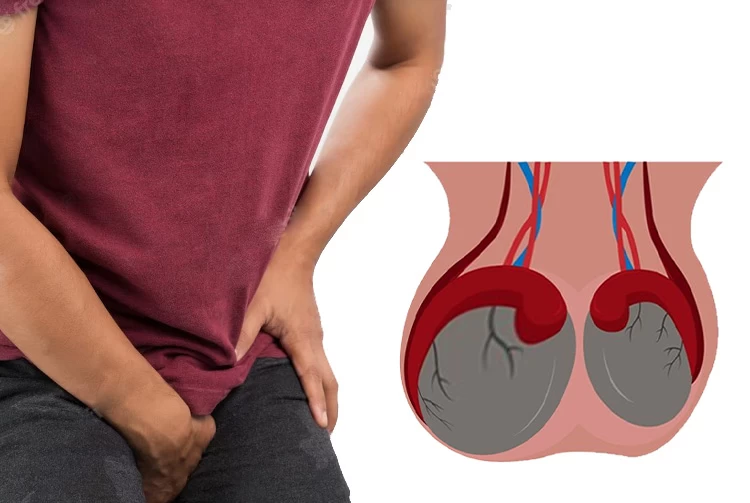
Varicocele (varicose veins): the most common testes disorder
Varicocele occurs when the veins in the scrotum are enlarged due to the blocked blood flow in the testes. This condition can sometimes be painful and affect male fertility. For this reason, men should have check-ups at least every 6 months and see a doctor if they see any bumps on the upper part of their testicles.
The occurrence of varicocele, especially grade-3 varicocele (the most severe), causes the shrinking of the testicles, increased testicular temperature, low spermatogenesis, and male infertility.
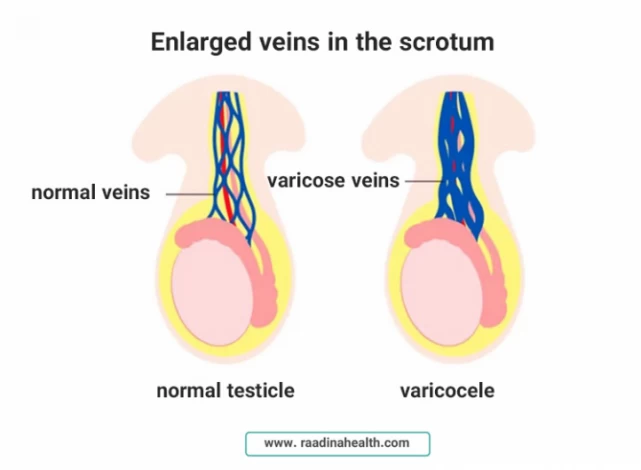
For varicocele treatment, there are some surgical and non-surgical procedures. One of the surgical options to treat varicocele is the microsurgical varicocelectomy which can ligate dilated testicular veins. Varicocelectomy can repair the damaged veins and correct the blood flow.
If the patient wants to have children, a semen test should be done every six months to check and treat male infertility.
Cryptorchidism (undescended testicle): a congenital anomaly
During pregnancy, the fetal testes are first located in the abdominal cavity and then migrate into the ducts and scrotum. Cryptorchidism occurs when the testicles do not descend and remain inside the abdomen after birth - especially in premature babies.
Men with undescended testicles may experience complications such as spermatogenesis disorders, decreased sperm number and quality, and male infertility.
Furthermore, the severe spermatogenesis disorder caused by undescended testicles can lead to genetic abnormalities and an increased risk of testicular cancer that cannot be treated even with surgery.
For cryptorchidism treatment, the baby's testicle should be moved from the abdominal cavity to the scrotum before month 12. However, surgery is needed in case of undescended testicle occurrence so the baby does not have sexual dysfunction and infertility.
Furthermore, as time passes, the density of germ cells (that produce sperm) decreases. Therefore, fertility potential can be preserved with timely orchiopexy before age 1.
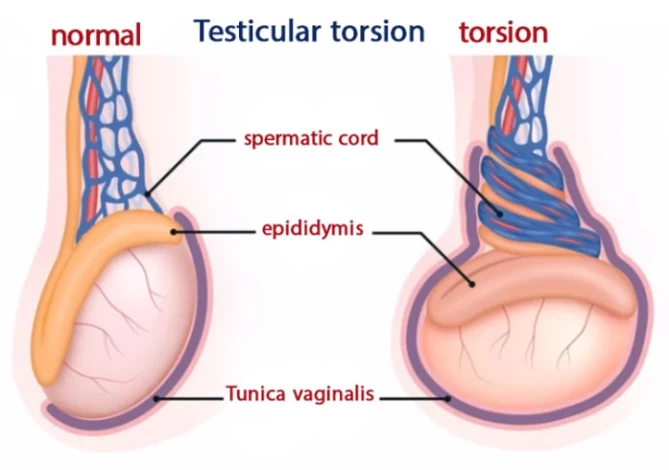
Testicular torsion, one of the testicular disorders in teenage boys
Testicular torsion occurs when the spermatic cord is twisted, preventing blood flow to the testicle. The condition is more common among teenagers and young adults. In testicular torsion, oxygen cannot reach the testicular tissues and cells and may cause the testicle to die.
Testicular torsion is one of the most dangerous testicular diseases that should be treated immediately. The reason is that if the torsion lasts more than a few hours - for a maximum of 4 hours - it can damage the testicular tissue and cause male infertility.
Surgery is required to treat testicular torsion by untwisting the spermatic cord.
Furthermore, a colour Doppler ultrasound can diagnose testicular torsion and reduce blood flow in the testis.
Testicular cancer
Testicular cancer is the most severe type of testes disorder and is also the most prevalent cancer among men aged 18 to 35, constituting 1% of all male cancer cases in the U.S. Fortunately, it is typically treatable.
Testicular cancer occurs due to conditions such as an undescended testicle, a family history of testicular cancer, and congenital abnormalities in the kidney and penis. This type of cancer usually affects only one testicle.
The healthy testicle is capable of producing testosterone for sperm production and pregnancy. If both testicles are affected by testicular cancer, it is possible to conceive by taking testosterone. Fertilization is possible two years after chemotherapy.
Testicular cancer is most common in young men between 30-35 years old. Therefore, paying attention to the symptoms and having a timely diagnosis helps treat testicular cancer and prevent its progression. Other symptoms of testicular cancer include pea-sized lump on bottom of testicle, swollen testicles, pain, heaviness in the testicles, lower abdominal and groin pain, and scrotal or testicular masses.
Testicular cancer is often diagnosed by finding a testicular mass or swelling. The most common treatment for testicular cancer is to remove the cancerous testicle and even some of the lumbar lymph nodes.
Although chemotherapy drugs may cause male infertility, it is recommended that patients store their sperm samples in the laboratory before chemotherapy treatment.
Testicular atrophy: an irreversible disease
Testicular atrophy is the shrinking of one or both testicles. The condition occurs due to factors such as getting mumps orchitis in childhood and using steroids in athletes.
However, as the scrotum controls the testicular temperature regulation, it sometimes becomes smaller or larger than normal due to decreased or increased temperature. Therefore, the change in the scrotum size should not be confused with testicular atrophy.
On the other hand, factors such as exposure to chemicals or testicular injuries can also cause the shrinking of the testicles.

Furthermore, testicular atrophy may increase the risk of abnormal sperm morphology and decreased sperm production due to low testosterone. Testicular atrophy is associated with complications such as teratozoospermia (sperm with abnormal morphology) and oligospermia (low sperm count) that can result in male infertility.
According to sources, testicular atrophy is irreversible and can only be prevented by managing its risk factors.
Epididymal cyst
An epididymal cyst (spermatocele or spermatic cyst) is a fluid-filled swelling in the epididymis. This condition often occurs due to sexual infections such as chlamydia and has symptoms like testicular pain, purulent swellings, and fever.
Epididymal cysts are common harmless complications that do not need any special treatment in most cases. However, they can be severe when they get large. In this case, the patients should see a urologist. If epididymal cysts are not treated, the scar created on the tissues blocks the reproductive tract over time and will cause male infertility.
Surgery is needed when the epididymal cyst becomes painful and extensive. However, this surgery can cause complications such as injury to the vas deferens or epididymis that will affect male fertility.
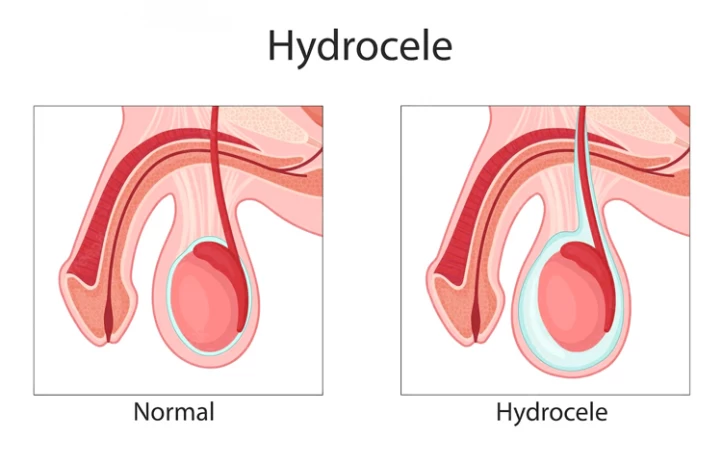
Hydrocele
Hydrocele is a fluid collection in the scrotum that is usually caused by an injury or trauma to the testicles. It is mostly benign. However, if the swelling becomes very large, it can cause symptoms such as testicle pain.
Hydrocele should not be confused with varicocele. Varicocele can cause male infertility, while hydrocele does not lead to fertility problems. Only if, in the case, the hydrocele is accompanied by underlying diseases such as the presence of a mass, tumor, or infection, it can cause low sperm count and will result in male infertility.
Surgery can be done if the hydrocele is large. In some cases, the non-surgical option is also performed by injecting a special substance into the scrotal wall to remove the hydrocele.
Hypogonadism
Primary hypogonadism occurs when the testicles do not produce enough testosterone. On the other hand, secondary hypogonadism is caused by a disease of the hypothalamus or pituitary gland.
Hypogonadism causes an increase in gonadotropin levels that will weaken sperm or lead to pituitary conditions such as prolactinoma and male infertility.
Hypogonadism symptoms include decreased libido, erectile dysfunction, development of male breast tissues, increased body fat, decreased muscle mass, reduced testicle size and strength, decreased body and facial hair, depression, and mood swings. According to research, various factors can cause hypogonadism, including undescended testicles, aging, taking chemical drugs, and diseases such as pituitary tumors, hemochromatosis, and Klinefelter syndrome.

The treatment of hypogonadism varies depending on its cause. If pituitary gland diseases cause the condition, pituitary stimulation increases testosterone and sperm production. Also, if this disease is related to the dysfunction of the testicles to produce testosterone, the testosterone replacement method (TRT) is recommended.
How to Diagnose and Prevent Testicular Disorders?
Men should check their testicles with special diagnostic methods at least every 6 months to prevent the development of testes disorders. For this purpose, the first step is to have a timely diagnosis. The doctor can detect testicular diseases by examining the history and measuring different body areas such as the testicles, scrotum, penis, and groin.
The next step is to prescribe helpful tests such as urine tests, semen analyses, blood tests, and cystoscopies.
Ultrasound is also done to determine the cause of the testicular condition more precisely in severe cases with the following methods:
- Testicular ultrasound is a non-invasive method that can examine the blood flow to the testicles and check anatomical disorders of the scrotum. Testicular ultrasound can diagnose testicular tumors, scrotum injuries, hematocele (accumulation of blood in the scrotum), epididymal cyst, and inguinal hernia;
- A testicular nuclear scan is a noninvasive method in which a colored radioactive material is injected into the vein. A change in the color of the affected part of the testicle indicates testicular torsion. However, nuclear imaging takes a long time in some hospitals and cannot be helpful.
When Is the Best Time to See a Doctor?
Since most testicular and scrotal disorders may lead to testicular swelling and pain, it is recommended that patients consult a specialist in case of any sudden pain, swelling, or changes in the testicle area. This will prevent the progression of the condition and help treat it.
It should be noted that diseases such as urinary tract infections (UTIs) and kidney and bladder stones can also cause swelling and pain in the area around the testicles. However, they are not among testes disorders.

Male Infertility Treatment in Iran
Iran's impressive progress in Types of Infertility Treatments during recent years has made this country a great destination for couples with fertility problems worldwide. Iran ranks first in the region with more than 70 high-equipped infertility centers. Also, due to the presence of skilled Iranian urologists, men with testicular disorders choose Iran as their medical destination. We at Raadina Health help you get the most effective infertility treatment in Iran at the most reasonable prices.
FAQs About Liposuction Aftercare
How do testes disorders affect male fertility?
Testes disorders can interfere with sperm production, quality, and hormone levels, leading to difficulties in getting pregnant.
What symptoms might indicate a testis disorder?
Symptoms of testes disorders can include pain or discomfort in the scrotum, swelling, changes in testicle size or shape, hormonal imbalances (like low testosterone), and male infertility.
Can testes disorders be treated?
Many testes disorders can be treated through medications, lifestyle changes, or surgery. The specific treatment may depend on the underlying condition and its severity.
What lifestyle factors can affect testicular health and male fertility?
Factors such as smoking, excessive alcohol consumption, drug use, obesity, poor diet, and exposure to environmental toxins can negatively impact testicular health, leading to male infertility.
Is it possible to father children if I have a testis disorder?
Many men with testes disorders can still father children, though it may be more challenging. Certain treatments and ART (assisted reproductive technologies) like IVF can be effective.




 WhatsApp
WhatsApp
 Telegram
Telegram
 Facebook
Facebook
 Email
Email












No reviews
Your comment