When Can I Breath Normal After Rhinoplasty Surgery?
Facial Plastic Surgery
Rhinoplasty, commonly known as a nose job, is a surgical procedure that reshapes the nose, often improving both its appearance and breathing function. While many seek the surgery for aesthetic reasons, regaining the ability to breathe normally after rhinoplasty is a common and equally important goal. However, the recovery process to restore normal breathing after rhinoplasty can differ greatly among patients. Some may find quick relief, while others might endure weeks or even months of adjustments before reaching ideal nasal airflow.
This article aims to provide a comprehensive understanding of the factors that influence breathing normally after rhinoplasty, shedding light on the potential challenges and offering guidance on how to navigate the recovery process.
We will explore the common causes of breathing issues after rhinoplasty, such as nasal valve collapse, septal deviation, and swelling. We will also delve into revision rhinoplasty, a procedure specifically designed to address breathing difficulties that persist after the initial nose job surgery. Additionally, we'll discuss preventative measures that can be taken to minimize the risk of breathing issues after rhinoplasty, ultimately ensuring a smooth and successful recovery journey.

Rhinoplasty and Its Impact on Nasal Breathing
Rhinoplasty surgery is a surgical procedure that aims to reshape the nose, enhance its appearance, and often improve breathing. While the cosmetic aspect of rhinoplasty is often emphasized, its impact on nasal breathing is equally significant.
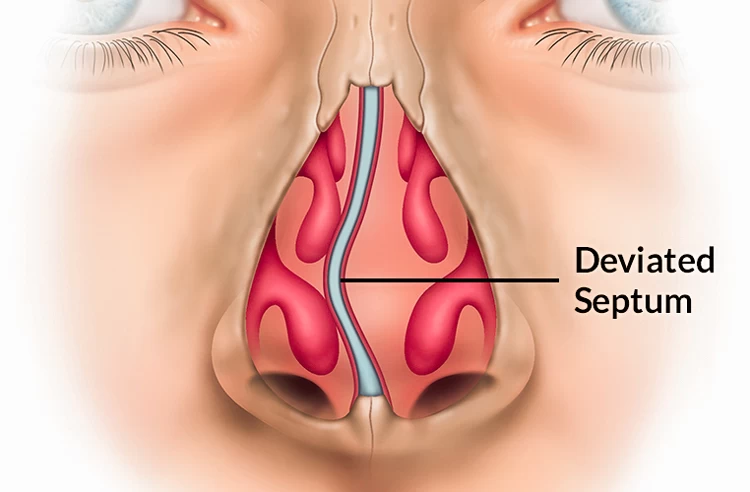
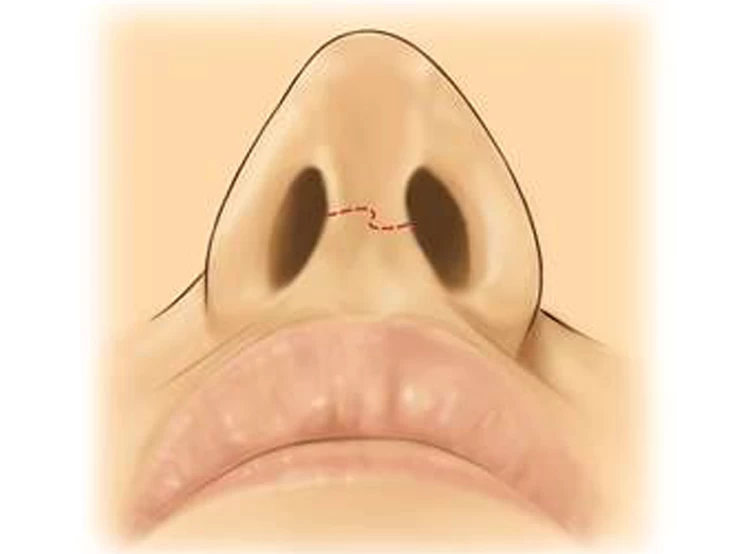
A well-executed rhinoplasty can address various breathing issues by correcting underlying structural problems. For example, a deviated septum, a crooked or misaligned nasal wall, can obstruct airflow and lead to difficulty breathing. Rhinoplasty can realign the septum, opening up the nasal passages and restoring proper breathing. Similarly, the procedure can address narrowed nasal valves, which are small openings at the entrance of the nasal cavity, and improve airflow by widening these passages.
However, it's crucial to acknowledge that rhinoplasty doesn't always guarantee improved breathing. Some individuals may not experience noticeable changes in their breathing, while others may experience temporary or even permanent breathing difficulties after rhinoplasty. This highlights the importance of choosing a skilled surgeon with expertise in both cosmetic and functional aspects of rhinoplasty.
Open communication with the surgeon is paramount before and after surgery. Discussing your breathing concerns and expectations with the surgeon can help in understanding the potential outcomes and managing any potential breathing issues after rhinoplasty.
When Can I Breathe Normally After Rhinoplasty?
Many patients experience some degree of nasal congestion and swelling, which can affect breathing after rhinoplasty. Typically, these symptoms begin to improve within the first week as the initial swelling decreases. By around one month post-surgery, most patients start to notice a significant improvement in their ability to breathe normally through their nose. However, it’s essential to remember that each person's healing process is unique, and factors such as the complexity of the surgery and individual anatomy can influence recovery time.
While many patients achieve a more normal breathing pattern within a few weeks, complete resolution of swelling may take 3 to 6 months. It's not uncommon for some residual congestion or altered airflow to persist for up to six months as the tissues continue to heal. Following your surgeon's post-operative care instructions and attending follow-up appointments will help ensure a smoother recovery and address breathing issues after rhinoplasty.
Timeline | Expected Breathing Changes | Key Considerations |
Immediately after surgery | significant nasal congestion, difficulty breathing through the nose, and possible nasal packing. | Swelling and packing may restrict airflow |
Week 1-2 | Nasal packing will likely be removed, leading to a gradual improvement in breathing. Swelling will begin to decrease. | Some discomfort and nasal dryness may persist |
Week 2-4 | Continued improvement in breathing as swelling reduces. | Most of the initial nasal congestion should have been resolved. |
Week 4-6 | Nasal breathing should be significantly improved. | Final results may not be evident for several months. |
Week 6-12 | Nasal breathing should be close to normal. | Swelling and bruising should be gone. |
Month 3-6 | Full recovery and normal breathing. | The final results will be apparent. |
Note: This is a general timeline, and individual results can vary.

Breathing Issues After Rhinoplasty
Rhinoplasty, or nose surgery, is a popular procedure designed to improve the shape and function of the nose. While it often achieves aesthetically pleasing results, some patients experience various changes, such as shortness of breath after rhinoplasty or even difficulty breathing after rhinoplasty. Most breathing problems after rhinoplasty are temporary and resolve as swelling subsides.
In the first 24 hours following rhinoplasty, patients often feel groggy due to anesthesia and may experience mouth breathing after rhinoplasty because of nasal congestion, facial swelling, and discomfort. The nose may be packed or supported with splints, impacting breathing after rhinoplasty. This initial stage is crucial for setting the tone for the rest of the recovery process.
The causes of difficulty breathing after rhinoplasty may include:
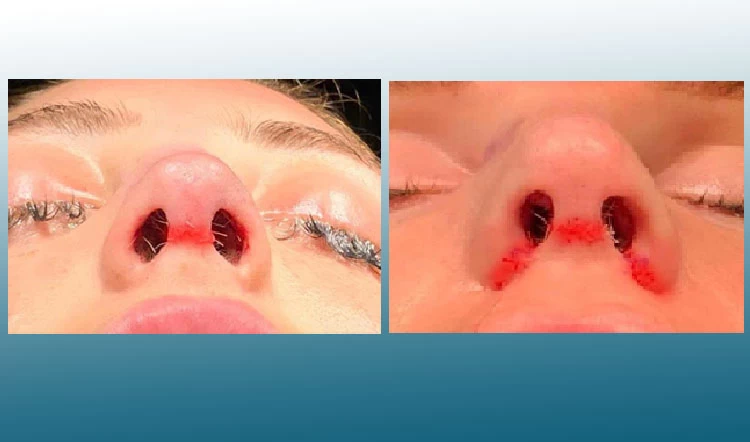
Uneven Nostrils after Rhinoplasty
Uneven nostrils are perfectly common after rhinoplasty. The nose may look asymmetrical due to the following problems.
- Excessive swelling inside the nose;
- The surgeon did the operation wrong and have damaged the nasal tissue;
- A pre-existing deficiency in the nasal structure;
- Wrong taping;
- Formation of a thick scar tissue inside the nostrils;
- Sutures have not been absorbed yet;
- Splints have been inserted wrongly or are removed too soon.
In any case, uneven nostrils can cause breathing difficulty and aesthetic problems. If the cause of nostril asymmetry is swelling, bad taping, or nonabsorbent sutures, it resolves within a couple of weeks without any treatment. However, if its cause is bad rhinoplasty, keloid scar, or a former problem with nasal bone, you probably need surgical treatment.
Dealing with Post-Surgical Swelling and Nasal Congestion
Swelling is a normal part of the healing process and can significantly contribute to breathing issues after rhinoplasty. Here's how:
- Nasal congestion: Swelling inside the nose can significantly narrow the nasal passages, making it harder for air to flow freely. This can lead to congestion, difficulty breathing, and a feeling of pressure or stuffiness;
- Internal Nasal Valve Swelling: The internal nasal valve is a crucial area for controlling airflow. Swelling in this region can cause it to collapse, further restricting airflow and making it difficult to breathe after rhinoplasty.
- Mucosal Inflammation: The lining of the nasal passages (mucosa) can become inflamed after surgery, adding to swelling and narrowing the airway.
- Mucociliary Clearance Issues: Swelling can impair the normal functioning of the cilia, which are tiny hairs that help move mucus out of the nose. This can lead to mucus buildup, further obstructing airflow and contributing to nasal congestion.
The swelling reduction timeline after rhinoplasty is a gradual process, with noticeable changes occurring over several weeks and months. In the first few days, expect significant swelling and bruising around the nose, eyes, and even the cheeks. Nasal tampons, typically removed within 2-3 days, will provide some relief in breathing.
As the first week progresses, swelling will start to decrease gradually, and the external splint supporting the nose will be removed after 1-2 weeks. While breathing becomes easier, some congestion and difficulty with nasal breathing may persist.
By weeks 2-4, swelling continues to lessen, but some residual swelling, especially in the tip and bridge of the nose, is normal. Breathing should be significantly improved, with less congestion.
Over the next several months, the swelling continues to subside slowly, with the majority of it gone by month 3-4. The final shape and contour of the nose start to become apparent. Breathing should be close to normal, with minimal or no congestion. While the majority of the swelling is gone, the final results of the rhinoplasty, including the full extent of breathing improvement, take about 6 months to reveal themselves fully.
Nasal Tampons and Splints after Rhinoplasty
Nasal tampons and splints are standard parts of rhinoplasty recovery, used to stabilize the nose and protect the surgical site. While essential for healing, they can also contribute to breathing issues during the initial recovery period.
While the nasal tampons are typically removed within 3 to 5 days after surgery, the external splint, which supports the newly shaped nose, will remain in place for about two weeks.
Once these are removed, you'll likely experience a significant improvement in breathing. However, remember that complete recovery, including the resolution of swelling and the healing of internal tissues, takes time. You can expect to experience some shortness of breath after rhinoplasty for approximately a month. This is normal and will gradually improve as your nose continues to heal.

Bad Nose Job Causing Breathing Problem
A poorly executed rhinoplasty can have serious consequences, particularly for breathing. If too much nasal tissue and cartilage is removed, the air passages become narrow, restricting airflow to the lungs. This can lead to chronic breathing difficulties after rhinoplasty, dry mouth, and even sleep apnea.
Beyond breathing issues after rhinoplasty, other signs of a botched nose job include:
- Nasal infections;
- A depressed nasal bridge (saddle nose deformity);
- Frequent nosebleeds;
- Uneven nostrils;
- Facial swelling;
- Loud breathing (stridor).
Fortunately, skilled rhinoplasty surgeons are trained to reshape the nose without causing lasting breathing issues. They focus on strategically repositioning the nasal structures rather than extensively removing cartilage. This approach minimizes the risk of long-term breathing problems.
While a botched nose job can often be corrected with procedures like cartilage grafting and filler injections, it's crucial to understand that healing is significantly slower in these cases due to scarring and tissue damage.
Ways to Relieve Nasal Congestion After Surgery
Here are some ways to relieve nasal congestion after surgery, focusing on methods that are safe and effective post-operatively:
- Saline Nasal Spray: The saline solution helps to thin out mucus, making it easier to clear the nasal passages. Follow your surgeon's instructions on how frequently to use the spray. It's generally safe to use frequently.
- Humidifier: Adding moisture to the air can help to loosen mucus and ease congestion. Run a cool-mist humidifier in the room where you're sleeping and resting.
- Nasal Corticosteroid Spray (Prescription): These sprays reduce inflammation in the nasal passages, helping to open up airflow. Only use these sprays as directed by your doctor.
- Elevating the Head: This position can help to drain mucus from the sinuses. Use an extra pillow or two when you're sleeping.
- Warm Compresses: Applying a warm compress to the forehead or sinuses can help to ease congestion and reduce pain. Use a warm, damp washcloth or heating pad, but avoid applying it directly to the surgical site.
- Avoiding Irritants: Exposure to smoke, dust, and strong scents can irritate the nasal passages and worsen congestion. Minimize exposure to these irritants as much as possible.
- Staying Hydrated: Drinking plenty of fluids helps to thin mucus and promotes drainage. Aim for at least 8 glasses of water per day.
- Over-the-counter (OTC) Decongestants: Oral decongestants can temporarily reduce swelling in the nasal passages. Use caution, as some decongestants may interact with certain medications or have side effects. It's important to discuss their use with your surgeon.
- Avoiding Blowing Your Nose Too Hard: Blowing your nose too hard can increase pressure and potentially disrupt the surgical site. Gently blow your nose, and only when necessary.
Managing Post-Surgical Swelling and Nasal Congestion effectively ensures a more comfortable recovery and contributes to the rhinoplasty's overall success. Patients must follow their surgeon's post-operative instructions and communicate any concerns regarding their recovery. If you want to know more about cleaning the nose after a nose job, read this article.
Revision Rhinoplasty: Correcting Post-Operative Breathing Problems
While rhinoplasty, or nose job, aims to enhance aesthetics, it can sometimes result in unintended breathing difficulties. Revision rhinoplasty focuses on correcting these post-operative issues, restoring proper airflow and improving the patient's quality of life. Whether it's that you can't breathe after rhinoplasty or other complications, this surgery requires meticulous planning and execution to restore nasal function and ensure patients can breathe normally after rhinoplasty.
Identifying the Need for Revision Rhinoplasty
Signs you might need a revision rhinoplasty may include:
- Persistent breathing issues;
- Unsatisfactory aesthetic outcome;
- Functional issues like whistling sound while breathing through the nose or recurrent nosebleeds;
- Persistent pain, discomfort, or swelling;
- Deformities or asymmetry.

Preventing Breathing Issues Post Rhinoplasty
Several steps can be taken to minimize the risk of breathing issues after nose job and ensure a successful surgical outcome, including:
- Thorough Consultation: Discuss your concerns and goals openly with your surgeon. Be upfront about any prior breathing issues or allergies you may have;
- Medical Evaluation: Ensure you undergo a complete medical evaluation, including a nasal endoscopy, to assess the structure of your nasal passages and identify potential risks;
- Experienced Surgeon: Choose a board-certified plastic surgeon specializing in rhinoplasty and with expertise in addressing breathing concerns;
- Strict Follow-Up: Adhere to your surgeon's post-operative instructions meticulously. This includes taking prescribed medications, keeping the surgical site clean, and attending all follow-up appointments;
- Avoid Smoking: Smoking can significantly impair healing and increase the risk of complications, including breathing problems;
- Early Intervention: If you notice any signs of breathing difficulties, such as congestion, difficulty breathing, or whistling sounds, report them to your surgeon immediately. Early intervention is crucial for addressing potential problems before they become severe.
Conclusion
While rhinoplasty can significantly enhance your appearance, it's essential to understand that the journey back to normal breathing can be a gradual process. Patience and meticulous post-operative care are key to achieving optimal results. While some individuals may experience immediate relief, others may need weeks or even months to regain full nasal function.
If you experience persistent breathing difficulties, don't hesitate to consult your surgeon for a thorough evaluation and necessary interventions. By following your surgeon's instructions and maintaining open communication, you can ensure a smooth recovery and achieve the desired outcome for both your appearance and your ability to breathe normally after rhinoplasty.
The insights and real patient experiences shared here serve as a valuable guide for those embarking on or recuperating from rhinoplasty. For more informative discussions and expert advice on similar topics, visit the Raadina Health Blog.
Rhinoplasty in Iran
Iran has become a global hub for rhinoplasty, attracting patients from around the world seeking skilled surgeons and competitive prices. The country has a well-developed medical tourism infrastructure, offering comprehensive services, including travel arrangements, accommodation, and translation support, making it convenient for international patients.
Iran boasts a large number of highly qualified and experienced plastic surgeons, many of whom have received training in renowned institutions around the world. Their expertise and artistic vision contribute to the impressive results achieved in rhinoplasty. Iranian clinics also utilize cutting-edge technology and techniques, including 3D imaging and minimally invasive approaches, to ensure precise and natural-looking results.
Moreover, compared to many Western countries, rhinoplasty costs in Iran are significantly lower, making it a financially attractive option for international patients.

FAQs About Breathing After Rhinoplasty
Why do some people experience breathing difficulties after rhinoplasty?
Breathing difficulties post-rhinoplasty often stem from swelling within the nasal passages, which can temporarily obstruct airflow. Structural changes during surgery, such as nasal septum or turbinate alterations, might also contribute to these issues. Generally, these breathing challenges improve as the swelling subsides during recovery.
What should I do if I encounter breathing problems after rhinoplasty?
If you experience breathing problems after rhinoplasty, consult your surgeon. They may recommend nasal saline sprays or steam inhalation to alleviate congestion. Persistent issues might require a medical evaluation to determine if further intervention is needed.
How long does the swelling last after rhinoplasty, and does it affect breathing?
Swelling after rhinoplasty is normal and can affect breathing. It typically peaks within the first week and gradually subsides over the following months. Most swelling resolves within a few months, but subtle changes can continue for up to a year.
Can overcorrection in rhinoplasty lead to breathing issues?
Yes, overcorrection in rhinoplasty, such as removing too much cartilage or excessively narrowing nasal passages, can lead to breathing difficulties. The surgeon must balance aesthetic goals with preserving structural integrity for optimal function.
What are the common risks or complications associated with rhinoplasty?
Common risks of rhinoplasty include bleeding, infection, anaesthesia complications, and dissatisfaction with aesthetic results. More specific complications can include difficulty breathing, nasal asymmetry, and needing revision surgery.
What's the typical recovery process for rhinoplasty, especially concerning nasal breathing?
Recovery from rhinoplasty usually involves initial swelling and discomfort, with gradual improvement in nasal breathing as swelling subsides. Most patients start feeling more comfortable within a couple of weeks, but it can take several months to a year for complete healing and final results.
How can I identify if my rhinoplasty results are not as expected?
Signs of unexpected rhinoplasty results include persistent nasal asymmetry, difficulty breathing, overly pronounced changes that don't look natural, or failure to achieve the desired aesthetic outcome. In such cases, consult your surgeon to discuss potential revision options.
Is revision rhinoplasty more complex than primary rhinoplasty?
Yes, revision rhinoplasty is often more complex due to the altered anatomy from the first surgery, scar tissue, and the need for precise corrections. It requires a surgeon with specialized expertise in revision procedures to address aesthetic and functional concerns effectively.
Can you breathe out from nostrils after a nose job?
Yes, but not immediately. After rhinoplasty, swelling and internal splints can make breathing through the nostrils difficult for the first 1–2 weeks. As the swelling subsides, breathing gradually improves, usually


























No reviews
Your comment